Journal of a Plague Year
“Pestilence is so common; there have been as many plagues in the world as wars, and yet both plagues and wars find people equally unprepared. The people of our town were no more guilty than anyone else…Why should they have thought about plague, which negates futures, journeys and debate. They considered themselves free, and no one will ever be free as long as there is plague, pestilence and famine.”
— Albert Camus, The Plague (1941)
Welcome to the University of Toronto Institute (IFP) for Pandemics data hub! This has been an extremely challenging year for all of us, but a small silver lining here at the Dalla Lana School of Public Health has been a generous donation from the Vohra Miller Foundation that has allowed us to open the IFP at the school. Why do we need an IFP? Aren’t there vaccines available for COVID-19? Isn’t there light at the end of the tunnel?
Thankfully, yes, even as we do see a terrible death toll around the world from COVID-19 (over 10,000 deaths a day at the time of writing), we do see hopeful signs on the vaccination front with the first Canadians vaccinated against COVID-19 this week. But the factors that created the conditions for this pandemic and a number of recent “near miss” epidemics (including the 2015 West African Ebola outbreak), including environmental degradation and climate change, massive global trade and travel, industrial agriculture and trade in bushmeat, risky laboratory research, and other factors, have not diminished or gone away. The toll in lives and economic damage wrought by the COVID-19 pandemic have demonstrated that investing in pandemic prevention, preparedness, control and resilience, all foci of the new IFP, is smart and necessary.
We have a number of excellent data resources for those wishing to understand the pandemic, that have been created by our colleagues at the University of Toronto, and many of those are already enumerated through the University of Toronto Map and Data Library. Our hope is that the IFP data hub will serve as an alternate, well curated clearing house for new epidemiological work on the pandemic, by ourselves at IFP and also by our colleagues at other Canadian and international universities.
With that in mind, let’s look back at some of the issues in the COVID-19 pandemic this week. Probably the most exciting development this week related to the use of the Pfizer-BioNTech (PBNT) vaccine for prevention of severe disease, here in Canada. The vaccine represents the first large-scale application of an mRNA vaccine in humans. What’s an mRNA vaccine? That’s a vaccine where your body is given the genetic code to make part of the virus (in this case something called “spike protein”) which you can then develop an immune response against. That immune response protects you from disease. We now know that the PBNT vaccine works VERY well; it reduces the risk of disease, and severe disease in those most at risk, by around 95%. That would have a huge impact on the pandemic here in Canada, if we could vaccinate enough people. And there’s the rub: everyone wants vaccine right now, vaccination takes time, and new vaccines like the PBNT and Moderna vaccines, need to be kept very cold; much colder than typical vaccines that can be stored in a standard fridge. But mRNA vaccines are an exciting new tool that will save many lives in the coming months, and which have huge potential for prevention of other diseases in the years ahead, including diseases with pandemic potential for which we lack vaccines.
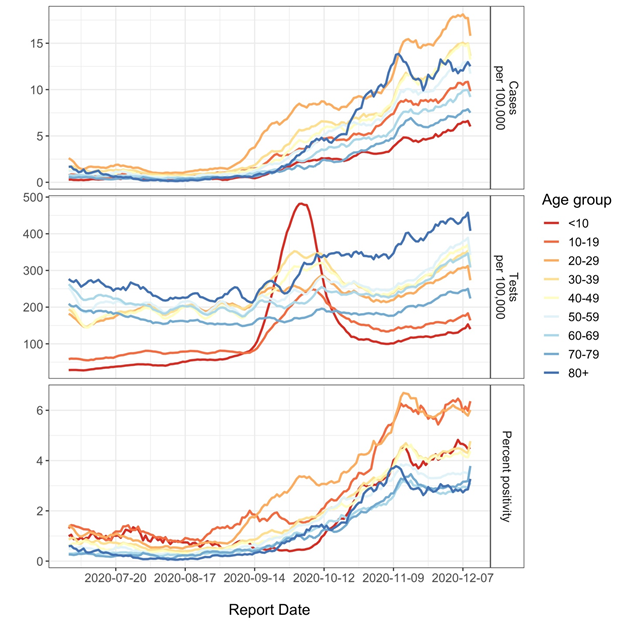
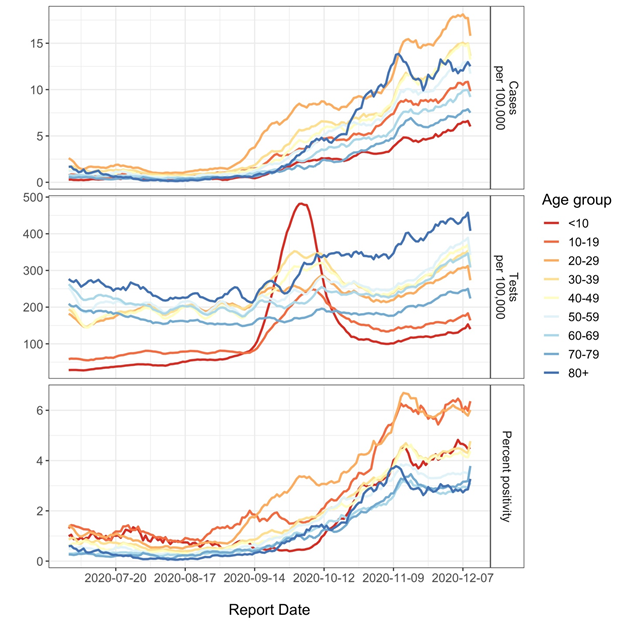
Here in Ontario, we see some positive developments resulting from increased restrictions on movement and mixing that probably result from areas with more active epidemics moving into the province’s “gray zone” category; that happened in Toronto and Peel back on November 23, and it takes a few weeks to see the effect of “lockdowns”. But we do now seem to be seeing a flattening of the “test positivity” curve in Ontario as a whole, and also in those two health units.
Lockdowns work (!) but they’re hard to sustain, and IFP researchers are continuing to focus on smarter, and more targeted, ways to limit COVID-19 transmission as we ramp up vaccination. One important area of study is the degree to which bioaerosols are responsible for the “superspreader events” that really drive explosive growth of COVID-19. Our University of Toronto engineering colleague Dr. Jeff Siegel was recently involved in a very cool study of a household in Texas in which an adult and child with COVID-19 were isolating. They found a lot of virus in the HVAC filter in the house, suggesting that it does, indeed, travel through the air. They also found virus on top of the TV and toilet tank; the top of the TV is a no-touch surface, which again suggests that airborne virus must have settled there. The top of the toilet tank is a reminder that “fecal aerosols” (microscopic poop-clouds!) may also be a mechanism for COVID-19 transmission. That’s got some very important implications for how we control COVID-19, both in the community, and in nursing homes and hospitals.
Lastly, we had a chance to think about the issue of COVID-19 in pregnancy this week. Emerging information suggests that pregnant women probably are at increased risk of severe outcomes from COVID-19, though we have no evidence that COVID-19 increases the risk of pre-term birth or stillbirth. The best way to protect pregnant women as we wait for vaccination? Keep transmission in the community as low as possible! My colleague Prof. Ashleigh Tuite and I wrote about this this week in the Globe and Mail, which published it through a partnership on science and society with the Royal Society of Canada.
Stay safe, stay distanced, wear your mask, and we look forward to talking to you next week!
