Brief on Primary Care Part 1: The Roles of Primary Care Clinicians and Practices in the First Two Years of the COVID-19 Pandemic in Ontario
Authors:Tara Kiran, Azza Eissa, Dee Mangin, Imaan Bayoumi, Noah Ivers, Sarah Newbery, Elizabeth Muggah, Jennifer Rayner, Dominik A. Nowak, Liisa Jaakkimainen, Michael Green, Susan Beazley, David M. Kaplan, Victoria Haldane, Andrew Pinto, Beth Cowper-Fung, Allan K. Grill, Nicolas S. Bodmer, Anna Perkhun, Roisin McElroy, Kamila Premji, Steve Nastos, Claudia Mariano, Onil Bhattacharyya, Sally Hall Dykgraaf, Michael R. Kidd, Rosemarie Lall, Katherine J. Miller, Onyenyechukwu Nnorom, Suzanne Shoush, Janet Smylie, James Wright, Richard H. Glazier, Fahad A. Razak, Karen B. Born, Danielle Martin on behalf of the Ontario COVID-19 Science Advisory Table
Key Message
Primary care is a critical entry point into both COVID-19- and non-COVID-19-related care in Ontario. Primary care clinicians (PCCs) played an integral and multi-faceted role in Ontario’s pandemic response. This included a rapid transition to virtual care; participating in testing, treatment, and wraparound services for COVID-19; providing education and support to local communities to increase vaccine uptake; and more recently, catching up with non-COVID care despite fixed resources. COVID-19 care is increasingly being integrated into primary care practices but without added resources or supports. At the same time, PCCs are supporting patients who experienced missed or delayed care through the pandemic. Practices funded to include interprofessional teams have inherently had more flexibility to support both the pandemic response and catch-up of non-COVID-19 care.
Summary
Background
Primary care offers a critical entry point into both COVID-19- and non-COVID-19-related care. PCCs have played an integral and varied role in the pandemic response in Ontario. Yet, many people across the province do not have a PCC or PCP (Primary Care Practice), leaving them without an important access point to comprehensive and continuous care. Further, access to primary care was often made more challenging during the pandemic. Ontario faces a significant challenge in keeping up with the demand for PCCs, both in pandemic waves to come and throughout health system recovery. Understanding the role of PCCs and practices during the first two years of the COVID-19 pandemic in Ontario is essential to improving our health care system and future pandemic preparedness.
Questions
In what ways have PCC workloads changed during the COVID-19 pandemic?
What has been the role of PCCs in the COVID-19 ‘test, trace, isolate, support’ response?
What has been the role of PCCs in COVID-19 vaccination efforts?
What has been the role of PCCs in delivering ongoing non-COVID-19 care during the pandemic?
How has virtual care been used by PCCs during the pandemic?
Findings
Across Ontario, PCCs have taken on additional roles to support COVID-19 care and ongoing routine clinical work. They have played an integral part in early 'test, trace, isolate, support’ efforts, primarily by supporting COVID-19 assessment and testing centres. Few, however, delivered these services in primary care clinics. As the pandemic progressed, PCCs have become essential in providing wraparound supports, remote monitoring, treatment, and support for people with post COVID-19 condition (long COVID). As vaccination efforts ramped up, PCCs were crucial in administering COVID-19 vaccines, largely in collaboration with hospital and community partners. Due to a variety of factors, only a small percentage of COVID-19 vaccination was delivered in PCPs. PCCs have been trusted sources of vaccine information, education, and outreach throughout the pandemic. PCCs worked with First Nations, Inuit, and Métis (FNIM) and Black-led community-based organizations, which have existing trusted relationships in structurally marginalized communities. These efforts focused on building trust in COVID-19 vaccines and contributed to a historic mobilization of resources to ensure that ‘no one is left behind’ in obtaining accurate pandemic information and receiving COVID-19 vaccination, testing, and care. Given the additive effect of COVID-19 demands, the clinical workload increased for many PCCs during the pandemic.
PCCs have responded to evolving clinical guidance and cared for patients contending with disrupted services throughout the pandemic. They were able to provide ongoing preventive, prenatal, well-baby, care of the elderly, chronic disease, and mental health care and addictions services, although there was variability in the ability to fully maintain pre-pandemic levels of care across these different domains. The use of virtual care accelerated and was positively assessed among most patients and PCCs; however, its use fluctuated with COVID-19 waves. Virtual care implementation has varied among clinicians and groups. Evidence is emerging on how best to integrate virtual care during the post-pandemic recovery phase in a way that is equitable, appropriate, and maintains comprehensiveness and continuity of care for conditions where in-person assessments are essential. Overall, PCCs continue to be challenged by balancing the new responsibilities related to COVID-19 while also ensuring provision of ongoing virtual and in-person routine PC services, in addition to mental health and complex chronic disease management.
Interpretation
Throughout the pandemic, PCCs played important roles in prevention, assessment, and management of COVID-19 while also supporting non-COVID care. PCCs have provided important wraparound supports for Ontarians, administered COVID-19 vaccines, leveraged trusting relationships to educate patients and the public, and collaborated with hospital and community partners to address critical equity gaps in communities across the province. These new roles resulted in trade-offs with non-COVID-19 care being deprioritized at times and some care gaps have emerged as a result. As the pandemic has continued, COVID-19-related work has increasingly been integrated into PCPs without additional supports or resources. PCCs with direct funding for interprofessional teams have inherently had more resources to support both COVID-19 and non-COVID-19-related care. In the current phase of the pandemic and beyond, the role of PCCs will be especially important given high levels of deferred care; long waits for specialty care and diagnostics; a rise in mental health and addictions issues; persistent gaps in health equity; and the need for clear communication to the public about how best to access the system and what to expect on the road to health system recovery. There is a need for definition and prioritization of roles of PCCs in relation to other parts of the health system in preparing for future pandemics and emergencies.
Background
Health systems with strong primary care achieve better health outcomes and improved health equity at lower cost.1–3 Primary care offers a critical entry point into both COVID-19- and non-COVID-19-related care by providing people with the “Four C’s” of first contact, continuity, comprehensiveness, and coordination.4 The international community has therefore repeatedly called for a focus on strengthening primary health care both in general, and in particular to support COVID-19 pandemic response and recovery.5–8
In Canada9 and internationally,10–15 primary care clinicians (PCCs) have played an integral and varied role in the pandemic response. The term “primary care clinicians” in this context refers to family physicians/general practitioners, primary care nurse practitioners, and other interprofessional health providers working in community health centres, primary care clinics, and teams in Ontario, including nurses, pharmacists, social workers, and others. Additional providers supporting primary care teams for First Nations, Inuit, and Métis (FNIM) communities may include Indigenous Cultural Service Providers such as Traditional Healers, Knowledge Keepers, Medicine People, Language Holders, and others.
Primary care spans the life-course, supporting preventive, prenatal, well-child, chronic disease, mental health and addiction, and elder care in an environment that must consider the specific circumstances, needs, values, and preferences of the person and family for whom they are caring. PCCs are central to the healthcare system, supporting patients to navigate and access specialized care and community-based interventions and supports. PCCs work in urban and rural communities as well as in long-term care, correctional facilities, homeless shelters, and academic settings.
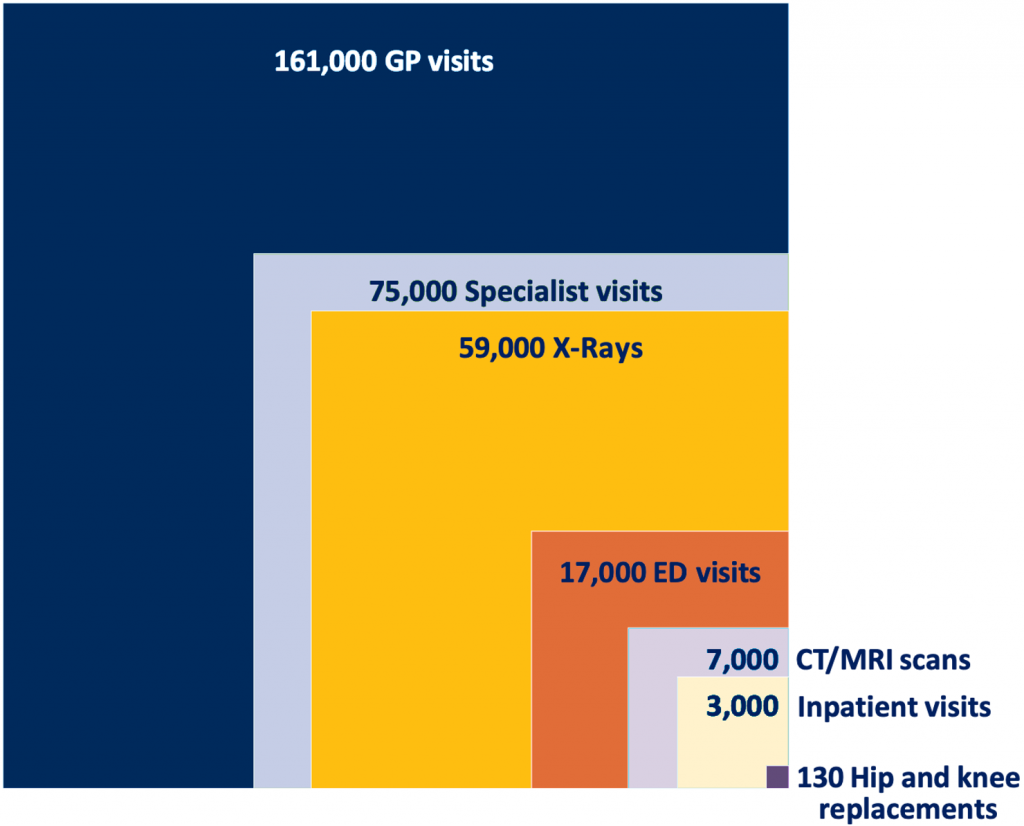
*Values rounded to the nearest thousand with the exception of hip and knee replacements, which were rounded to the nearest 10. Adapted from Ontario Medical Association, OMA Economics, Policy and Research slide-deck.20 Data source: 1) OHIP Claims FY2019 2) CIHI National Ambulatory Care Reporting System FY2019 – Ontario only 3) CIHI Discharge Abstract Database FY2019 – Ontario only.
GP, general practitioners and family physicians. ED, emergency department. CT, computed tomography. MRI, magnetic resonance imaging.
PCCs often support upstream efforts to address health disparities with an equity-lens that considers the social determinants of health.16
Ontario, with its population of over 14.8 million people and projected growth of 5.6 million people over the next 25 years,17 has a large and growing demand for primary care. On any given day, many more Ontarians need to access a primary care clinician than hospital or specialist services (Figure 1).18,19 Indeed, Ontario faces a significant challenge in keeping up with demand for primary care at baseline, but also in potential pandemic waves to come and throughout health system recovery.
Understanding the role of PCCs during the first two years of the COVID-19 pandemic in Ontario is, therefore, essential to improving our health care system and future pandemic preparedness. This Brief explores the ways in which PCCs workloads and roles have changed across the COVID-19 response, COVID-19 vaccination efforts, and in delivering ongoing preventive care and care for conditions other than COVID-19 during the pandemic. This Brief reflects mainly on the role of family physicians and general practitioners during the pandemic, as data on other PCCs and practitioners is lacking and/or emerging. Most data currently available relates to larger urban and/or academic PCPs; hence important contributions of community-based practitioners are likely underrepresented. Additional information and analyses on the roles of non-physician clinicians in primary care, such as nurse practitioners and physician assistants, are needed.
Questions
In what ways have PCC workloads changed during the COVID-19 pandemic?
What has been the role of PCCs in the COVID-19 ‘test, trace, isolate, support’ response?
What has been the role of PCCs in COVID-19 vaccination efforts?
What has been the role of PCCs in delivering ongoing non-COVID-19 care during the pandemic?
How has virtual care been used by PCCs during the pandemic?
Findings
In What Ways Have PCC Workloads Changed during the COVID-19 Pandemic?
In Canada9 and internationally,10–15 PCCs have played integral roles in the pandemic response. Clinically, this has included:
- COVID-19 assessment, testing, and isolation support
- Vaccination counselling and delivery
- Therapeutic prescribing and/or referral
- Post COVID-19 condition diagnosis, management, and care
- Health Human Resources (HHR) support in other sectors, particularly during surges (e.g., staffing Emergency Departments, Intensive Care Units, and Long-term Care Homes)
- General support, education, and counselling of patients related to COVID-19 and system navigation
- Maintenance of non-COVID-19 care
In addition, primary care organizations with access to interprofessional teams have redeployed staff to ensure ongoing support for people experiencing loneliness, mental health challenges, and impacts of increased poverty, food insecurity, and other determinants of health.21 PCCs also took on new non-clinical roles. For example, in many regions, the pandemic sparked or accelerated collaboration and information sharing between primary care clinicians. These informal networks could collectively respond to new pandemic demands in collaboration with hospitals, long-term care, public health, paramedic services, and social care.22–25
Across all major PCP models, including the Family Health Organization (FHO), Family Health Group (FHG), Comprehensive Care Model (CCM), and Fee for service (FFS), the number of days worked by PCCs significantly increased in 2020 compared to 2019 (Figure 2).
In Ontario, 48% of Ontario family physicians billed an hourly sessional code related to work done in COVID-19 assessment and vaccination centres in fiscal year 2021.26 COVID-19 responsibilities have most often been in addition to ongoing routine clinical work. For example, between February and October 2021, all Ontario family physicians billed a mean of 45 assessment centre units (corresponding to approximately five hours per month, likely representing both vaccination and testing centre work).27 During the same period, total primary care visit volumes (not including assessment centres) remained at pre-pandemic levels.28,29
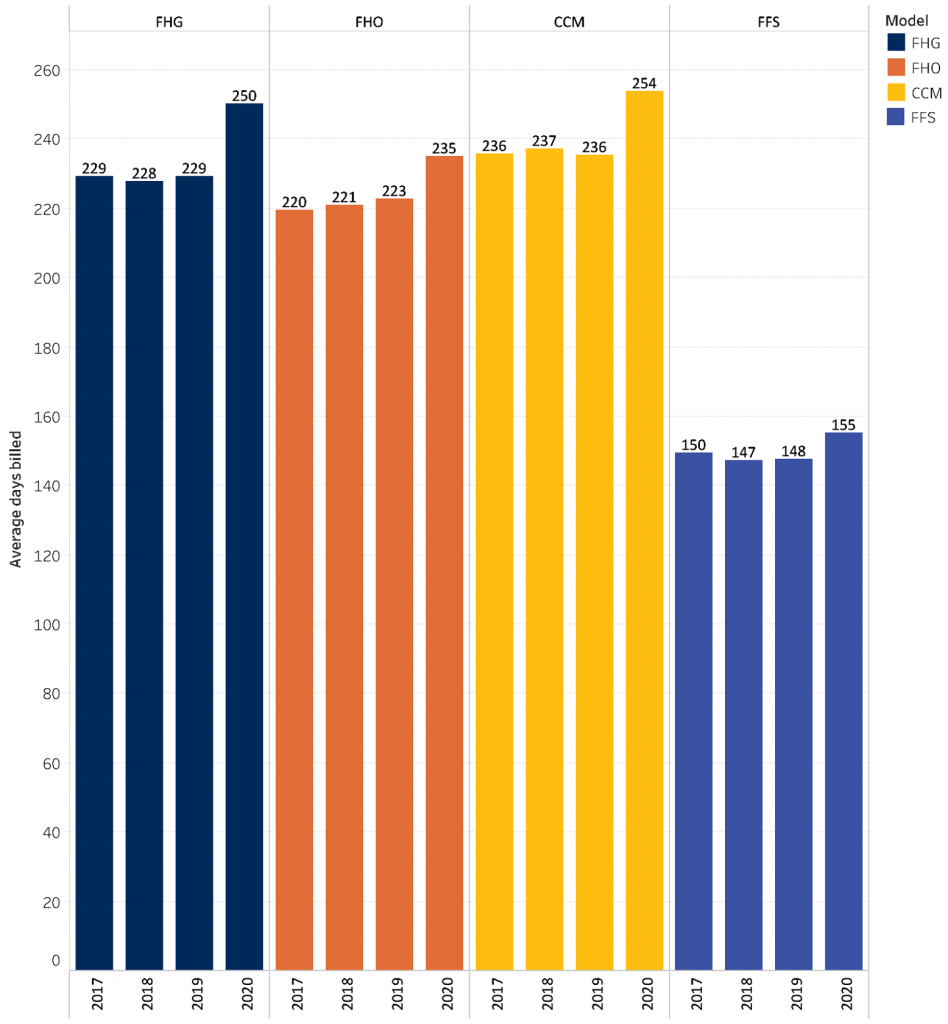
FHO, Family Health Organization: physicians formally enroll patients, are largely paid by capitation, and may or may not have funding for an interprofessional team.
FHG, Family Health Group: physicians formally enroll patients and are largely paid by fee-for-service with a small amount paid via capitation. They work in groups of three or more physicians.
CCM, Comprehensive Care Model: physicians formally enroll patients and are largely paid by fee-for-service with a small amount paid via capitation. They do not work in groups.
FFS, Fee-for-service: physicians do not formally enroll patients and all payment is by fee-for-service.
What Has Been the Role of PCCs in the COVID-19 ‘Test, Trace, Isolate, Support’ Response?
PCCs integrated emerging evidence throughout the pandemic and played an integral role in providing COVID-19 assessment, testing, and wraparound supports for people who needed to isolate or quarantine, as well as offering remote monitoring, treatment, and support for people who had persistent post-acute symptoms. PCCs provided trusted education to their patients throughout the pandemic and helped clarify changing public health messages.
COVID-19 Assessment, Testing, and Contact Tracing
The primary care workforce supported testing at designated COVID-19 assessment centres (including drive-through and mobile clinics) and via community outreach in a range of settings including homeless shelters, retirement homes, long-term care, and community-based clinics, as well as for homebound seniors.30However, during the first year of the pandemic, only a minority did in-person COVID-19 assessment and/or testing in the primary care office. Barriers to testing and assessment in the office included concerns for patient and staff safety, physical space constraints, workflow challenges, and early in the pandemic, availability of personal protective equipment (PPE). In contrast, clinic testing was more feasible when there was a collaboration or affiliation with the local Public Health Unit (PHU) or hospital. In some regions, such as Ottawa and Kingston, PHUs supported family physicians to dispense take-home PCR tests to their patients directly, and patients could return these to a lab near them (Michael Green, personal communication).
A January 2021 survey of Toronto-area family physicians found that 30.8% of PCCs reported seeing patients who had symptoms consistent with COVID-19 in their offices.31 Among those who provided in-person care to symptomatic patients, 69.5% were in a Family Health Team (FHT), even though FHT doctors made up 40.8% of the physicians in the study. In comparison, non-FHT Patient Enrolment Models (PEM) (FHO, FHN, FHG) made up 46.9% of physicians in the study but accounted for only 18% of those providing in-person care to symptomatic patients. Size of the physician group was also an important indicator of willingness to provide in-person care. Regardless of the payment model type, 80% of physicians providing in-person care practiced in a group setting with more than five physicians, although these large groups made up only 53% of all physicians. Non-physician providers in Community Health Centres (CHCs) and Nurse Practitioner-Led Clinics (NPLCs) were also active in assessing, testing, and contact-tracing structurally marginalized patient populations and continued to provide information, see symptomatic patients, and provide in-person care.21
Contact tracing was considered a cornerstone of the early COVID-19 response. However, by fall 2020 many PHUs were unable to effectively contact trace due to staffing strain.32 Collaboration with primary care for contact tracing was not a feature of Ontario’s pandemic response, nor does it appear to have featured prominently in primary care in other jurisdictions.13
There were early reports of culturally unsafe contact tracing experiences reported by members of the FNIM community in Ontario, including experiences of racism and microaggressions when contacted by contact tracers.33 In response, the Indigenous Primary Health Care Council (IPHCC), in collaboration with the Ministry of Health, created a training program titled “Contact Tracing: Inspiring Cultural Safety in Indigenous communities” to support the implementation of Indigenous-specific contact tracing across the province.34 The 40-minute course was developed to provide contact tracers and case investigators with the necessary tools to support culturally safe interactions when contact tracing in Indigenous communities. To date, the course has been completed by approximately 1057 individuals.
Finally, PCCs provided considerable education and support to patients and the public related to testing, isolation, and contact tracing both through individual encounters and through sharing information in newsletters, websites, social media, and traditional media. This was particularly important during the Omicron wave when public health no longer had capacity to follow up with individuals diagnosed with COVID-19.35 For example, the ConfusedAboutCOVID.ca website was co-developed by the Ontario College of Family Physicians and Department of Family and Community Medicine at the University of Toronto to provide clear information on COVID-19 and vaccines to the public from a trusted source. It launched on January 12, 2022, during the height of the Omicron wave in Ontario, and by February 8, 2022, the site had 32,464 total page views and 35,769 total PDF downloads (Allison Williams, email communication).
Wraparound Supports
Wraparound supports for COVID-19 are services that meet the complex health and social needs of people needing to isolate or quarantine. While many PCCs supported COVID-19-positive patients during quarantine and isolation, this depended on available clinic resources. Team-based practices, such as FHTs, NPLCs, and CHCs, have nurse practitioners, social workers, nurses, and other health professionals, as well as community ambassadors. Thus, through their structure, they inherently had significantly greater resources and flexibility to provide wraparound supports. For example, social workers, health promoters, and dietitians were able to connect people to community resources including mental health supports.30
Innovative care models to deliver wraparound supports extended the reach of primary care into communities during the pandemic. Such models ranged from virtual reality programs to help isolated seniors, proactive wellness checks of vulnerable adults, new models of mental health care, and many more.36–38 Indeed, over half of FHTs reported providing care to individuals who were not their regular patients and over half reported involvement in COVID-19 response regional planning (Association of Family Health Teams of Ontario, personal communication). Both CHCs and other PCPs connected with COVID-19 isolation hotels and homeless shelters, as well as farms to reach migrant workers.38,39 Indigenous-led models were developed to serve the particular needs and concerns of urban Indigenous communities. For example, the “Call Auntie” program in Toronto developed services in response to emerging needs covering public health, clinical, and logistical areas related to health, within a decolonized framework that used a range of staff beyond traditional clinicians (Suzanne Shoush, personal communication).
Remote Monitoring
Many PCCs and PCPs supported patients with COVID-19 to safely recover in the community through clinical care and remote monitoring housed in primary care across the province.40 Programs were supported by Ontario Health and Hamilton Family Medicine, who together, through the primary care COVID@Home clinical pathway and support program, facilitated PCC access to oxygen monitors, evidence-based clinical pathways, electronic medical record (EMR) tools and education via a community of practice.40 Through the primary care pathway, selected patients were provided with home oxygen saturation monitors, actively monitored by the clinic during their illness and given advice about management of other chronic conditions and medications during their illness. Lower-risk patients were given illness management advice, isolation support and instructions on when to call the clinic for further support.
Data collected from PCCs associated with the primary care COVID@Home clinical pathway estimate these programs reached a practice population of over 7.6 million people.41 Participating PCPs were predominantly interprofessional care teams (80.4%), and most (90.3%) were in urban settings.41 Within participating practices, health professionals took on different roles. In some models, nurses would do phone assessment and counselling, consulting physicians as needed, while in others, physicians played a more primary role. Social workers provided help navigating resources or mental health supports, and in 2022, pharmacists could support decision-making regarding therapeutics.
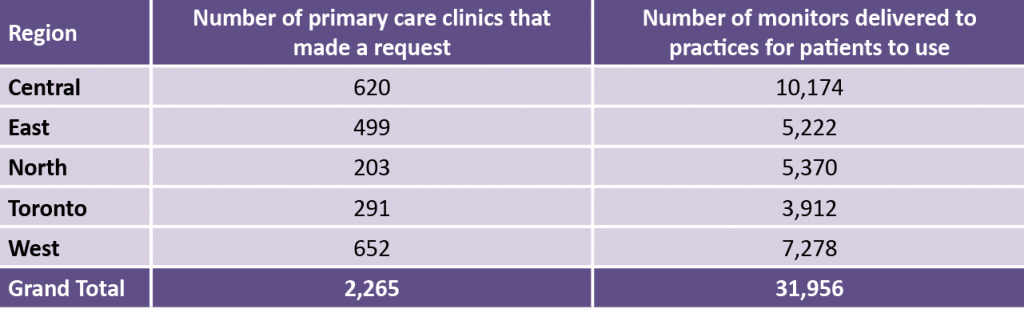
Table 1 below describes the reach of the pulse oximeter supply for the COVID@Home clinical pathway. These coverage data offer a conservative estimate; many practices implemented the program independently, as they already had their own supply of monitors. The model was rolled out across Ontario on March 1, 2021. In the 12 months that followed, there were 19,474 unique users in Ontario of the clinical pathway on the hfam.ca website.
Implementation of the COVID@Home clinical pathway for acute care of COVID-19 by primary care with supporting resources facilitated rapid and equitable reach of COVID-19 care across the province and was associated with improved patient outcomes and high patient satisfaction.41 Available mortality data suggests better patient outcomes among those accessing COVID@Home services when compared with population data for Ontario. In a prospective cohort study, data on outcomes for all patients monitored by primary care using the COVID@Home clinical pathway were collected from 147 of the PCCs implementing the COVID@Home (n=4556 patients). In this cohort, mortality was significantly less (0.4% mortality vs 0.9% (p<0.001)) than that found in a retrospective population-based cohort study of people in Ontario who tested positive for COVID-19 carried out during the same time period and in the same population (non-Long Term Care) (Dee Mangin, personal communication).
Treatment
Shortly after the approval of Paxlovid treatment by Health Canada, Paxlovid prescribing and dispensing was opened up to PCCs and pharmacists to enhance access and potentially improve equity for rural and marginalized communities.
As of September 8, 2022, approximately 85% of Paxlovid prescriptions dispensed at a pharmacy were prescribed by a PCC with 81% prescribed by a family physician (FP) or general practitioner (GP) and 4% by a nurse practitioner (NP); over 7,500 FP/GPs and 560 NPs have prescribed at least one course of Paxlovid. Note that this analysis is based on prescription claims data submitted from community pharmacies and excludes courses dispensed at a clinical assessment centre or in hospital (Daniel Warshafsky, email communication). This achievement has been facilitated by multiple factors, including:
- Publicly-available expert guidance on Paxlovid from the Ontario COVID-19 Science Advisory Table42
- Timely continuing professional development43 and resource compilation44
- Collaboration with community pharmacists
- Availability of Paxlovid prescribing tools that could be integrated into commonly used electronic medical record (EMR) systems45
- Having in-house pharmacist expertise for those in team-based models
- Specialist or pharmacist consultation in some COVID-19 clinical assessment centres
- Patient communication supports developed by Ontario Health and others46
The central role of PCCs in Paxlovid prescribing in Ontario illustrates the relative efficiency of rapidly implementing new clinical guidelines by PCCs when the health system efficiently uses communication and support pathways in primary care. Factors that contributed to this were new partnerships, pathways, and approaches that were put in place in previous pandemic waves as a result of learnings from the early days of COVID-19 assessment and vaccine rollout. Data on the proportion of eligible patients for Paxlovid actually receiving treatment should be used prospectively to identify potential gaps in matching therapy to need.
Post COVID-19 Condition Support
Studies estimate that as many as 10 to 15 percent of people with COVID-19 will have symptoms lasting longer than 12 weeks (known as “post COVID-19 condition” or “long COVID”),47,48 although this proportion is likely to be lower in a population with a high level of immunity as currently exists in Ontario. Current evidence suggests that most adults with post COVID-19 condition can be diagnosed and managed in primary care, especially given the need for longitudinal follow-up.48 Frontline PCCs support assessment and counselling for post COVID-19 condition and can help navigate social supports, including paperwork for disability claims or other forms of financial compensation. PCCs can also draw on government guidance49 and specialist advice, for example, via e-consultation.50 As with other aspects of COVID-19 prevention and management, clinicians working in team-based settings have additional supports to draw on for these patients including mental health, pharmacist, and sometimes rehabilitation supports.51 The magnitude and scope of primary care work related to post COVID-19 condition are currently difficult to accurately ascertain, given there is no specific billing code for the condition. Likewise, quality of care for the post COVID-19 condition is currently difficult to assess.
What Has Been the Role of PCCs in COVID-19 Vaccination Efforts?
Across Ontario, PCCs have supported vaccination efforts not only by administering the COVID-19 vaccines, but also by being trusted sources of information regarding vaccine efficacy and side-effects, providing ongoing education for vaccine-hesitant patients, and supporting equitable access through collaborative outreach with CHCs and community ambassadors with trusted existing relationships in marginalized communities. Ontarians who did not have a regular family doctor were less likely to be vaccinated. Research analyzing vaccination in Ontario prior to September 1, 2021, found that 39% of people without a regular family doctor were unvaccinated (having zero doses of any COVID-19 vaccine) compared to only 19% of people with a regular family doctor.52
Administering COVID-19 Vaccines
In Ontario, PCCs administered the COVID-19 vaccines in a variety of settings outside their primary care offices, including mass immunization clinics, community-based pop-up and mobile clinics, and hospital-based clinics. Administration of the COVID-19 vaccines in primary care offices was limited during the initial 1.5 years of the vaccine rollout. Primary care offices contributed the most to vaccination of younger children, who were approved for COVID-19 vaccines much later (November 2021 for children ages 5 to 11, and September 2022 for children 6 months to 4 years).
Figures 3 illustrate the proportion of vaccines delivered in various settings in Ontario between December 2020 and mid-August 2022, stratified by local PHU providing the vaccine (Figure 3a), as well as by person’s age and dose received (Figure 3b). Overall, 4% and 3% of the first and second vaccine doses were administered in primary care offices. The largest contributions (6% first dose and 6% second dose) were for children ages 5 to 11 years old (Figure 3b), compared to 2% first dose and 2% second dose in adolescents ages 12 to 17 years old, and 4% first dose and 3% second dose adults 18 years and older. The overall proportion of vaccines delivered in primary care offices varied by PHU from 1% (e.g., Brant, Chatham-Kent) to 11% (Grey Bruce). However, publicly available data on vaccine uptake suggest no correlation between PHUs with a higher proportion of delivery by primary care clinics and overall uptake.53
Ontario’s PCP vaccine delivery largely began with the primary care pilot initiated for the AstraZeneca vaccine in March 2021. A wide range of innovative strategies, including drive-through and pop-up clinics, were employed to maximize efficiency and reduce risk. Team-based PCPs had pharmacists, nurses, and other staff providing additional support for in-house primary care office delivery. However, even at the time of the pilot, only 16% of the 190,000 doses of AstraZeneca vaccine went to primary care offices, even though the AstraZeneca vaccine could be stored in the fridge at 2-8+ °C, like many of the routine vaccines delivered in primary care offices (Dominik Nowak, personal communication). The pilot was further complicated by reports of adverse events related to the AstraZeneca vaccine54 which may have undermined momentum for office-based vaccination.
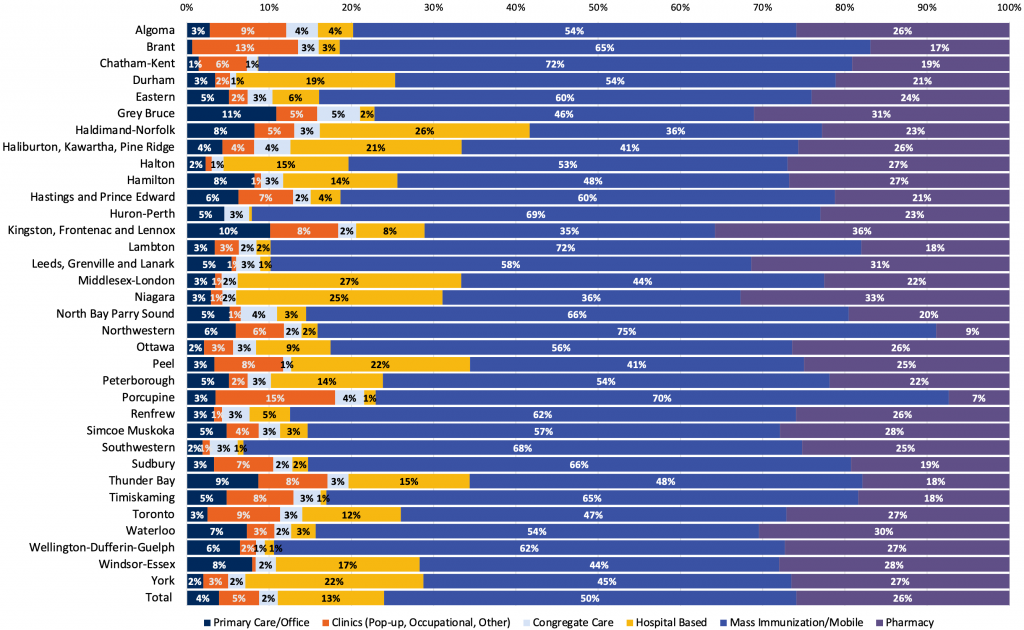
Source: Ontario Ministry of Health data received via personal communication from D. Warshafsky on Aug 11, 2022.
Mass vaccination clinics played an important role during initial stages of the pandemic, and Canada has notably high first and second dose vaccine uptake relative to peer countries. However, the sustainability of vaccination efforts more broadly would likely be strengthened by better integrating vaccinations in primary care, for example, to increase the uptake of booster doses which have had relatively low uptake in Ontario. PCCs have historically provided most vaccinations in Canada in their primary care offices. The low rate of COVID-19 vaccine delivery in primary care offices in Canada is in contrast to other jurisdictions, such as the UK, where more than two-thirds of vaccinations were delivered in primary care offices.55
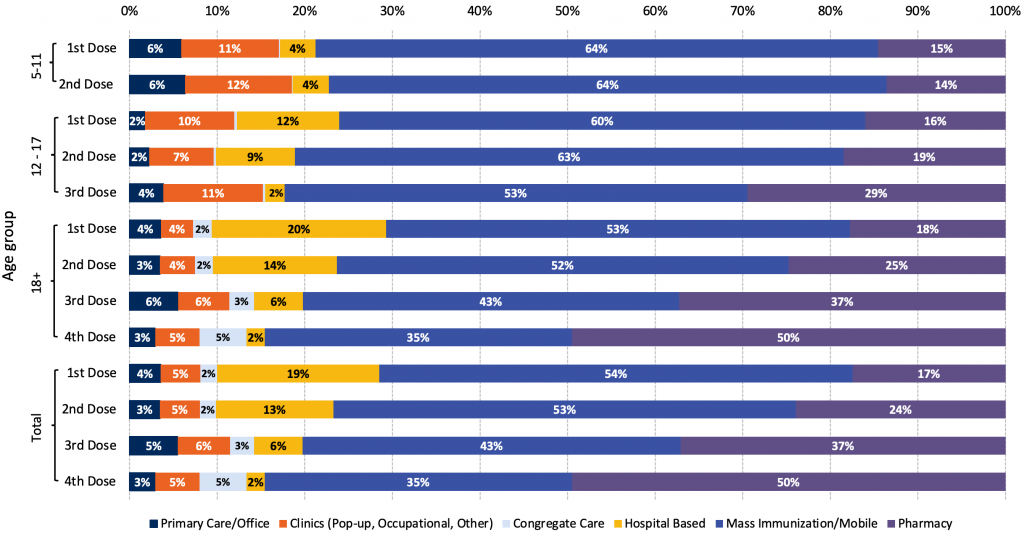
Source: Ontario Ministry of Health data received via personal communication from D. Warshafsky on Aug 11, 2022.
The absence of primary care representation on the provincial COVID-19 Vaccine Distribution Task Force may have affected the extent to which the design of the primary care vaccine rollout was effective in engaging and supporting office-based immunization.
Factors driving low vaccine delivery by primary care offices have not been robustly studied. Anecdotally, several intersecting factors contributed to low delivery even when vaccines were available. These included supply chain management, information technology challenges, resource constraints, and incentivization toward providing vaccines outside of PCPs. Early in the COVID-19 vaccine rollout, there were strict storage requirements for mRNA vaccines, a limited and unpredictable supply, and a focus on mass vaccination clinics and distribution to pharmacies. Currently, significant issues remain, such as short duration of vaccine stability and the size of the multi-dose vials distributed as the size curtails PCC ability to perform opportunistic vaccinations (the norm for primary care) without substantial wastage. Further, the COVID-19 vaccine information system, COVaxON, was noted to be an additional barrier by some PCCs given time demands for user registration requirements, lack of integration with existing patient medical records, and a cumbersome user interface. Clinics and providers have also reported other resource-related challenges including physical space, competing clinical priorities, and health human resource shortages. In addition, well-compensated OHIP billing codes to vaccinate patients in mass vaccination clinics may have further disincentivized PCCs from providing COVID-19 vaccines in their own clinics. These clinics provided a relatively high hourly rate which was originally introduced to support work in assessment centres at a time when COVID-19 testing was considered risky. The same rate, however, was used to compensate for work in vaccination centres; work that was lower in risk and complexity. More study is required to better quantify barriers to COVID-19 vaccine administration in primary care offices to support sustainable vaccine rollout for future rounds of boosters or newer vaccine modalities.
Compared to Ontario, other Canadian provinces started their vaccine rollout earlier (Quebec and Nova Scotia on March 1, 2021, vs. Ontario on March 15, 2021) and placed a greater focus on a centralized vaccine booking and documentation system (Clic Santé in Quebec and CANImmunize in Nova Scotia) to streamline community-based vaccine access and delivery. Nova Scotia’s CANImmunize, has been well-perceived by both patients and clinicians as efficient and user-friendly,56 potentially contributing to a higher vaccination rate.57
Building Trust in COVID-19 Vaccines
Vaccine hesitancy was a concern in all Canadian provinces, with over 9% of adult Canadians declaring no intention to vaccinate based on a nationwide survey of COVID-19 vaccination intention.58 For many, PCCs are a trusted source of health information given ongoing relationships developed over time. Trust is one of the most important determinants of vaccine uptake,59 and across Ontario, PCCs have been trusted sources of information in an evolving landscape of vaccine misinformation and disinformation. Indeed, polling done by the Ontario College of Family Physicians (OCFP) early in the COVID-19 vaccine rollout found that 83% of patients ranked family physicians as the most trusted professionals, that the family physician’s office was the most preferred setting for vaccine delivery, and that people who were unsure about the vaccine were more likely to say yes if the vaccine was endorsed and delivered by their family physician.60
Clinicians build trust through effective communication, in addition to demonstrating care and competence.61Provision of trusted advice requires that PCCs have confidence in being able to answer typical questions from patients about COVID-19 and vaccination. Multiple strategies were employed to address this gap. For example, the OCFP and the University of Toronto Department of Family and Community Medicine (DFCM) held webinars every two weeks that brought primary care experts and specialists to speak on current issues challenging PCCs in their management of COVID-19. In total, these were attended live by over 4,200 unique PCCs, with 65% attending multiple sessions and additional PCCs watching the archived recordings.43 The OCFP and DFCM also produced a self-directed e-learning series available free online that was completed by over 4700 individuals.62
Providing COVID-19 Vaccine Education and Enhancing Outreach
PCCs have been able to provide important COVID-19 vaccine information not only through individual counselling of patients but also through mass communication to practice populations, thus extending their outreach and offering opportunities for patients to seek their advice.63,64 Proactive outreach to under-vaccinated patients was supported by audit and feedback reports provided to family physicians in enrolment models by Ontario Health.65 Reports provided patient-level COVID-19 vaccination data from COVaxON, but required additional work for PCCs to reconcile. Use of COVaxON was therefore made easier in team-based models that had the support of data specialists. Unvaccinated patients were not distributed evenly across PCPs. An analysis of administrative data found that a disproportionate number of unvaccinated Ontarians clustered within a relatively small proportion of PCPs (Noah Ivers, personal communication). Further research is underway to better understand the factors influencing this variation, but it seems one factor is that these physicians were less likely to belong to a team than physicians with fewer unvaccinated patients. Ontario Health worked with primary care leaders to implement targeted practice facilitation to support PCPs with greater needs and fewer resources.66
Individual and practice-level efforts to build vaccine confidence were supported by several factors, including timely continuing professional development,43,62 timely e-consultation services,67 and pharmacist collaboration, particularly in models where pharmacists are part of the team. Additionally, some family physicians partnered with community health workers and/or medical students to enable patient outreach related to vaccines.68
Primary care leaders also spearheaded communication to the public, for example, through social media, newsletters, local media, and websites like ConfusedAboutCOVID.ca. There were also new collaborations to support evidence-based communication and information to the public. Family physicians, pediatricians and other PCCs worked with the Kids Come First OHT (kidscomefirst.ca) and the Children's Hospital of Eastern Ontario (CHEO), for example, to open a COVID-19 Care Clinic for children and youth.
The Alliance for Healthier Communities worked with 12 community-based primary care organizations (11 CHCs and one FHT) to build upon the trusted relationships they had with their communities and implemented innovative methods of promoting vaccine confidence in marginalized communities with long histories of mistrust. As of June 2022, this initiative has supported the vaccination of 15,000 people.69
Community Outreach and Enhancing Equity
Worldwide, the COVID-19 pandemic in all its dimensions, including incidence, testing, and severity, has been associated with social inequalities.70–74 The pandemic disproportionately impacted FNIM, Black, and racialized people, and marginalized communities living in Ontario.75–78 These communities also tend to have poorer access to a regular PCC.79–81 Targeted strategies were needed to support these communities in relation to COVID-19 assessment, management, and support. Community-based strategies to support early pandemic response and vaccination among marginalized groups were particularly important, given high rates of mistrust due to historical and present-day racism and colonialism perpetrated by the medical and scientific community.82,83
Many FNIM peoples have a deeply rooted fear and distrust of clinicians and the health care system due to the ongoing impacts of colonialism. To build trust in COVID-19 vaccines and vaccine administrators, the IPHCC focused efforts on building the cultural safety capacity of PCCs and other clinicians. In collaboration with the Ontario Medical Association (OMA), IPHCC presented a “Wise Practices Webinar” to identify wise practices and strategies for working in a culturally safe and respectful way when providing COVID-19 vaccinations to FNIM people. The IPHCC developed the “6 Steps to Effective Engagement for Vaccine Distribution with FNIM Peoples” engagement guide to support culturally safe and accessible vaccination.84
FNIM community members required priority access to vaccines in part due to higher incidences of COVID-19 illness and hospitalization compared to the non-FNIM population.85 PCCs and specific community services serving FNIM and Black communities co-lead a historic mobilization of resources to address pressing mistrust of COVID-19 vaccines and needs in these communities in collaboration with community and hospital partners.30 For instance, “Operation Remote Immunity” was highly successful in supporting timely vaccination of FNIM communities in remote Northern Ontario, where primary care access is particularly limited.86,87However, vaccination of FNIM living in urban and related homelands lagged.88 Indigenous community leaders, health and social service providers, and PCCs (including Indigenous midwives, nurses, and physicians) brought attention to the importance of equitable geographic distribution and access to vaccines and rapidly implemented Indigenous-led vaccine initiatives to increase outreach and accessibility.
Data from a March 2021 Statistics Canada survey showed that only 57% of Black Canadians reported willingness to receive the COVID-19 vaccine compared to 77% of the overall population.89 Black PCCs from various clinical and social settings partnered with CHCs (such as the TAIBU CHC and Black Creek CHC), supported by the province’s High Priority Communities Strategy, their community ambassadors, key partners from the Black Health Alliance, Black Scientists’ Task Force on Vaccine Equity, Black Physicians’ Association of Ontario (BPAO), and many others to address this issue. As a result of these partnerships, they co-hosted successful Black-led vaccine pop-up and wellness clinics that enhanced vaccine uptake in ‘hot-spot’ areas in Toronto and cities across Ontario.90 Black-led partnerships with FNIM leaders and allies also resulted in resources to provide mentorship to medical learners, residents, and colleagues who did not have expertise in working with Black communities (e.g., the OMA module on addressing vaccine distrust among Black people).
In addition to the collaborative equity-focused efforts above, PCCs led vaccination efforts in shelters, among people recently incarcerated, undocumented residents, migrant workers, as well as elderly living in long-term care homes, retirement homes, or who were homebound.30 Each of these efforts required unique approaches and collaborations. Efforts were also supported through innovative collaborations between groups. For example, FNIM PCCs were consulted when wellness and pop-up clinics serving Black and racialized communities were established; BPAO provided outreach to other marginalized communities, including international agricultural workers, uninsured people, homeless populations, and people who had been in the prison system. The community outreach and equity partnerships helped to build trust and reciprocity and instill confidence in COVID-19 vaccines and will likely further support marginalized communities during COVID-19 recovery.91
What Has Been the Role of PCCs in Delivering Ongoing Non-COVID-19 Care during the Pandemic?
In addition to new care responsibilities directly related to COVID-19, PCCs in Ontario have been supporting ongoing “routine” non-COVID-19 care throughout the pandemic. This includes providing care for patients impacted by restricted hospital services, as well as providing preventive, chronic, and acute care in a range of settings, such as the office, long-term care, patients’ homes, shelters, and more. The type and amount of care often shifted because of directives from the Ministry of Health and the trajectory of the pandemic.
Responding to Shifting Priorities through Changes in Volume and Type of Care
Early in the pandemic, primary care was instructed to defer all non-essential in-person care to limit COVID-19 transmission, preserve PPE, and allow for redeployment of health care workers into COVID-19 programs. Total visit volumes decreased overall. Reassuringly, total visits declined the least among those with highest health care need.92 By fall 2020, overall total visits had risen back to pre-pandemic levels (Figure 4a). However, patterns differed by age group. In the first two years of the pandemic, total visit volumes were below pre-pandemic levels for children (Figure 4b).
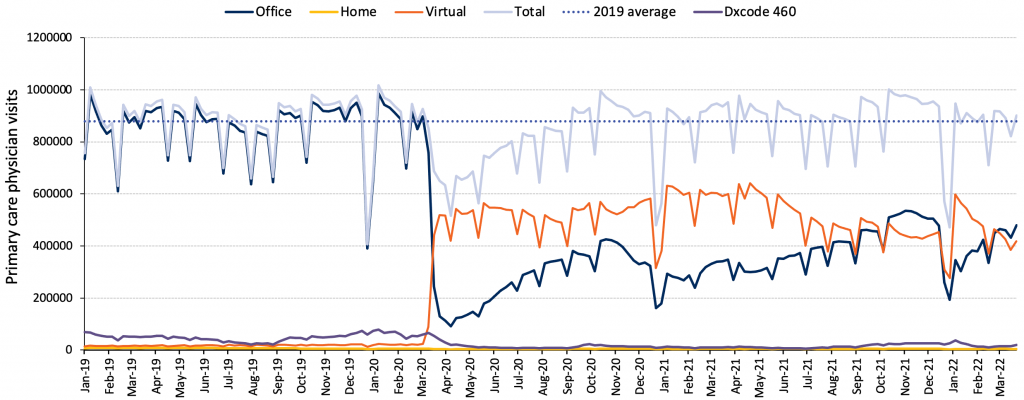
Source: Unpublished data from INSPIRE-PHC using data from ICES provided by Kiran et al.27
The reduction in total visits for children may be related to the decrease in non-COVID-19 viral illnesses that usually bring this population to the primary care clinic (Figure 4b). In contrast, total visit volumes were above pre-pandemic levels for those 75 and older (Figure 4c). This finding among older adults is in keeping with research showing relatively high visit rates for people living with Parkinson’s disease and dementia.93 The initial drop in in-person visits and pivot to virtual care was a global phenomenon in primary care.94
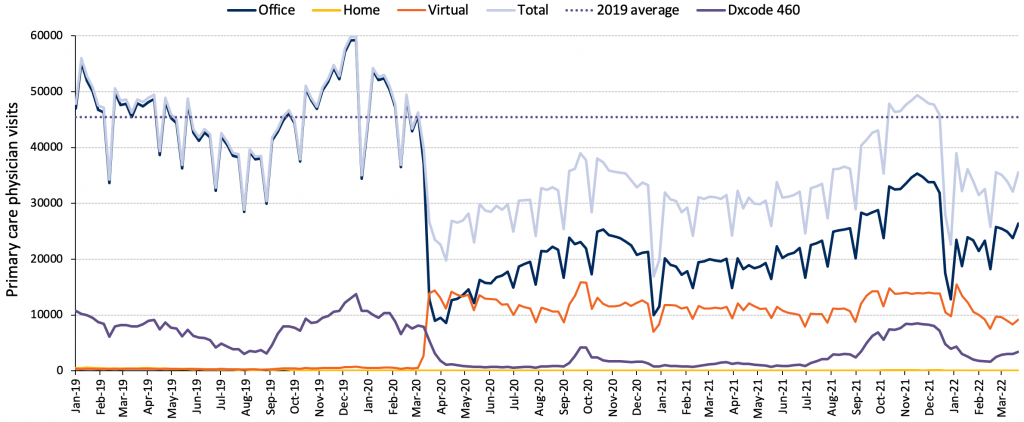
Source: Unpublished data from INSPIRE-PHC using data from ICES provided by Kiran et al.27
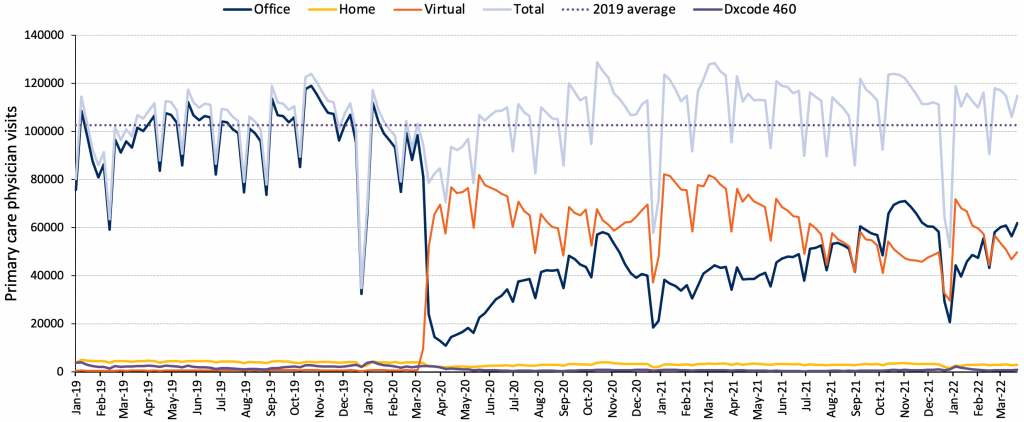
Source: Unpublished data from INSPIRE-PHC using data from ICES provided by Kiran et al.27
One reason for reduced visit volumes was patients themselves deferring care. In one survey, almost one-third of patients reported delaying seeking care during the first few months of the pandemic. A higher proportion of those with trouble making ends meet and those with lower self-rated health reported delays in seeking care.95
Providing Care for Patients Awaiting Disrupted Surgeries and Services
Across pandemic waves, care needs in communities have been affected by difficult decisions to restrict hospital services in response to waves of COVID-19. Delaying some surgeries and services had ripple effects felt not only in hospitals but in primary care. In Canada, the duration of restricted hospital services was 63 days (from March 17 to May 19, 2020) compared to a 46-day average duration of restriction among 28 European countries during the first wave. In turn, patients needing non-essential surgeries and services relied on PCCs for ongoing care and symptom management.
Providing Preventive Care
Primary care is an important site for the provision of preventive care in communities. While emerging analysis suggests that many non-COVID-19 primary care services were maintained in Ontario throughout the pandemic, some preventive care fell behind, including non-COVID-19 vaccinations and cancer screening. This may partially be due to PCCs being instructed during the early part of the pandemic to defer preventive care and focus on COVID-19 assessment, testing, and essential care. However, this would not explain persistent deficits at late stages of the pandemic.
The volume of primary vaccinations for infants and babies up to and including age 1 year stayed at pre-pandemic levels throughout the pandemic (Figure 5a). However, routine vaccinations for those 4 to 6 years of age dropped dramatically and do not seem to have caught up. Reasons are multifactorial; however, a major driving factor was likely the suspension of vaccine mandates for school-age children. Other potential reasons include prioritization by clinicians and decisions by parents to defer immunization especially given the wider age range that was acceptable, as well as fewer in-person visits for that age group leading to fewer chances for opportunistic vaccination.
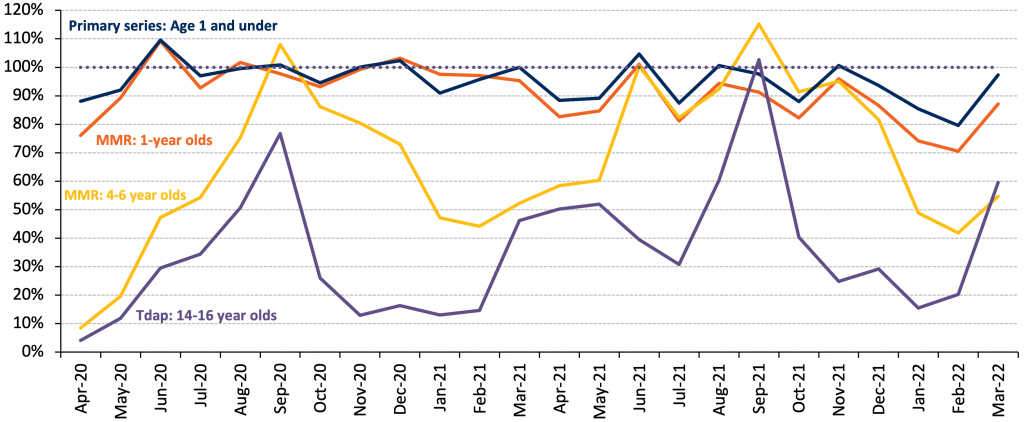
Source: Ontario Health via personal communication from Ismail Z.
There was also a drop in cancer screening rates. The proportion of Ontario residents eligible for cervical, colorectal, and breast cancer screening who were up to date dropped from 60%, 66% and 61% to 50%, 61%, and 48%, respectively, between October 2019 and October 2021 (Figure 5b). Fortunately, catch-up is underway. Testing volumes for Pap tests to detect cervical cancer, fecal immunochemical tests (FIT) to detect colon cancer, and mammograms to detect breast cancer have risen by 32%, 52%, and 15%, respectively, comparing winter 2021/22 with pre-pandemic levels in 2019.96 Testing volumes reflect contributions from many parts of the system including backlogs at mammography centres and laboratories processing FIT tests. Efforts are underway to encourage prioritization of “high impact" preventive care,97 particularly given that in order to address the backlog in care, rates would need to exceed pre-pandemic levels. Equity-related gaps in cancer screening were an issue pre-pandemic,98,99 and research is needed to understand whether these gaps have widened and, if so, how these gaps should be addressed.
Other high-income countries also observed rapid declines in cancer screening and referrals for cancer treatment, including in the United Kingdom, the United States, and Australia.7 While such restrictions may have been beneficial in terms of pandemic control, the population-level health impacts are not yet known. There is clear evidence that even short delays in initiation of cancer treatment are associated with increased mortality.100
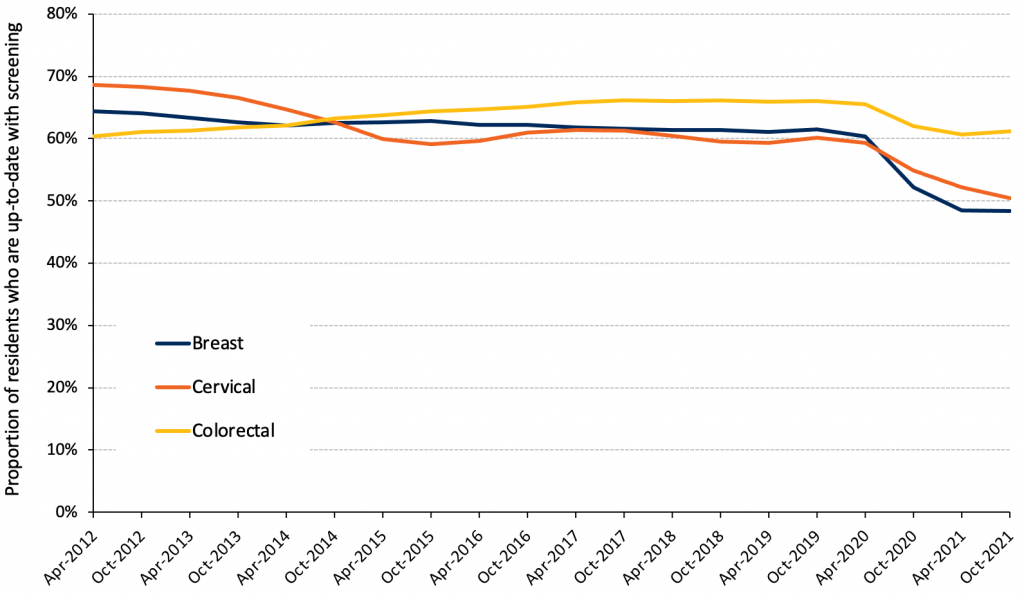
Source: Unpublished analysis of ICES data from INSPIRE-PHC. Lofters et al.101
Providing Care for People Living with Chronic Disease, Mental Health, and Addictions
Despite primary care and health system responses to increase access through virtual care (discussed later in this Brief) and other innovations, people with chronic conditions have been particularly impacted by delayed care. Often this was because they were reluctant to visit health care settings in person, for example, due to fear of being infected with COVID-19. Many countries observed increased mortality over pre-pandemic levels, outside of that due to COVID-19. While some may be misclassified as COVID-19-related deaths, some were related to opioid overdoses, and others may have been related to deaths from chronic conditions.102,103 By October 2021, Ontario experienced a 6% increase in mortality over pre-pandemic rates of which 86.5% were COVID-19 related.104 In England, non-COVID-19-related mortality among people with diabetes was 11% higher than pre-pandemic and was highest among those who did not complete diabetes care processes in the preceding two years.105
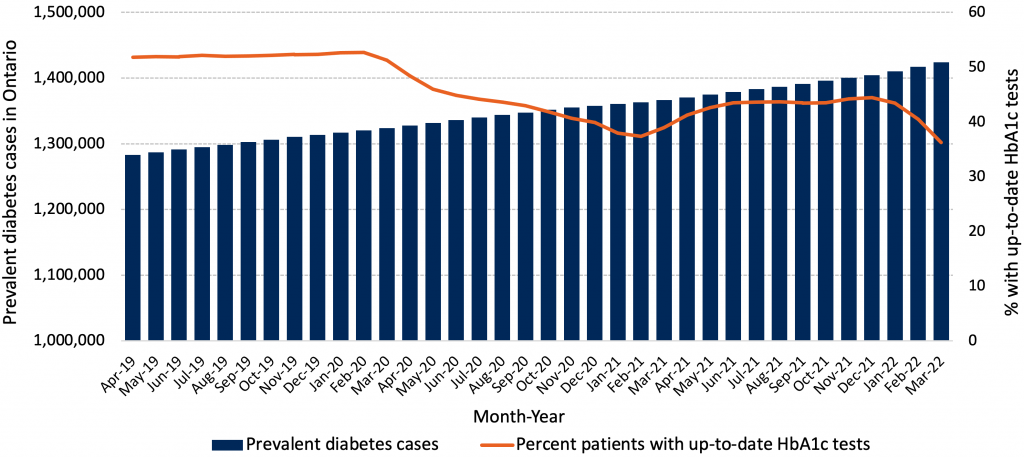
Although overall visit volumes returned to pre-pandemic levels within six months, there is evidence across health systems of delayed diagnosis and delayed care. In Ontario, by March 2022, approximately 35% of people with diabetes had two or more glycated hemoglobin tests in the last year, compared with 50% in 2019 (Figure 6). Part of the decline can be explained by guidance to reduce frequency of testing in patients whose values had previously been stable and within target,106 but some likely relates to inadvertently missed care. Internationally, there is also evidence of reduced new diagnoses. The number of patients with a first diagnosis of six chronic diseases (hypertension, hyperlipidemia, diabetes mellitus, depression, heart disease, and congestive heart failure) was reduced by 30-40% in the first pandemic wave in the United States and subsequently returned to baseline.107
The diagnostic backlog also impacts other vulnerable populations, such as older adults. Overall primary care visit volumes for older adults with dementia or Parkinson’s disease had rebounded by the end of the first wave, with the majority of care delivered virtually.93 However, preliminary findings demonstrated a significant reduction in dementia diagnosis, triggering important questions about the appropriateness of virtual visits for older adults with complex needs.108
Finally, the pandemic has seen a rise in mental health concerns and substance use, including increases in self-reported symptoms of depression, anxiety, and increased use of substances (smoking, alcohol, and non-prescription opioid use).109–112 PCCs are often the first point of access for these conditions, and a substantial proportion of PCC visits are related to a mental health or addiction concern.113–116 PCCs were able to access some new virtual mental health supports that became available during the pandemic, including Wellness Together Canada and time-limited virtual Cognitive Behavioural Therapy services.117 However, only a minority of PCCs work in teams that include publicly funded social workers or psychologists. Many were left supporting patients to recover and navigate supports on their own.
How Has Virtual Care Been Used by PCCs during the Pandemic?
During the pandemic, use of full virtual consultations and remote monitoring became widespread in primary care. This was driven by a need to reduce physical contact, the advent of new billing codes, and infrastructure investments. The expansion of virtual care modalities and billing codes enabled both continuity of non-COVID-19 care, as well as the rapid scaling of COVID-19 triage, monitoring, and early detection of serious illness within comprehensive primary care practices, based on existing evidence-based models of extended primary care.118,119 Net new virtual care in Ontario was overwhelmingly done by telephone.95
In the first four months of the pandemic, virtual primary care increased dramatically, comprising 71.1% of primary care physician visits.92 The proportion of care delivered virtually subsequently decreased and then fluctuated. Higher rates of virtual care coincided with higher COVID-19 case counts in the community,29suggesting the possibility of both patient and provider preferences for socially distant, non-contact care during surges. The proportion of care delivered virtually has also varied by physician, group, and rurality.29,92
By March 2022, 46% of care was virtual (Figure 4a). This is comparable to many non-procedural medical subspecialties. In fiscal year 2021, Ontario rheumatologists provided 36% of visits virtually, gastroenterologists 44%, neurologists 39%, while psychiatrists provided 55% of visits virtually (Ontario Medical Association, personal communication). A small number of family physicians practiced almost entirely virtually. Between Feb and Oct 2021, only 400 family physicians (2.6% of all family physicians) had 100% of visits that were virtual.29It is not known what the ideal proportion of virtual visits should be in primary care, but it is unlikely that managing all patients virtually would provide high-quality care.
Initial research suggests positive experiences with virtual primary care among many patients. For example, in one Ontario survey of 500 primary care patients, respondents overwhelmingly reported that telephone/video visits reduced time (97% / 97%), costs (81% / 85%) and were more convenient than in-person care (91% / 91%).120 The majority wanted telephone (69%) and video (71%) visits at least as often as in-person visits post the COVID-19 pandemic, while only 5% did not want any future virtual care.120 In a survey of over 7500 patients in the Greater Toronto Area (GTA), respondents reported high levels of comfort with all virtual modalities; 75%, 52% and 43% of respondents said they wanted their practice to continue offering phone, email/secure messaging, and video after the pandemic, respectively.95
Digital equity was challenged due to multiple factors, including lack of devices, inadequate access or reliability of data/Wi-Fi, comfort in use, and not being in culturally safe environments. A recent study conducted with CHC patients and clinicians suggested that while the transition to virtual delivery of care had removed some access barriers, including cost and transportation, the need for technology had created new barriers. In the GTA survey, patients who reported difficulty making ends meet, those new to Canada, and those with fair or poor health reported lower comfort with virtual care and were less likely to want virtual care options to continue.95 However, preferences for and equitable access to virtual care are complex and influenced by multiple contextual factors. Some studies have shown that despite equity concerns and implementation challenges, patients and clinicians alike voiced preference for continuing the option of virtual visits for specific aspects of their care, even among more marginalized groups.121,122
The use of virtual care continues for many reasons, including convenience, efficiency, ease of access for clinics and patients, and commercial opportunities for for-profit groups. The impact depends on how it is integrated within primary care. For example, a year and a half into the pandemic, there were concerns that some family physicians were providing too much care virtually and that this was causing increased demand in the emergency department. However, research has found that at a population level, physicians who provide more virtual care did not have higher emergency department visit rates among their patients compared to those who provided less virtual care.29 In contrast, some commercial ventures provide virtual “walk-in” care without the option of in-person assessments or a longitudinal primary care model, which can lead to fragmentation of services and possibly draw family physicians away from comprehensive primary care.123Unfortunately, poor continuity of care and the lack of physical examination may be contributing to increased emergency department utilization by virtual walk-in clinic patients. Research has found that virtual walk-in patients are both less likely to have a subsequent in-person physician visit and twice as likely to have a subsequent emergency department visit within 30 days (8.3% vs. 4.1%) compared with patients having a virtual family physician visit.124
The way in which virtual care has been integrated into PCC practice has changed during the pandemic. Early in the pandemic, PCCs were instructed to take a virtual-first approach to care. This approach meant PCCs were encouraged to assess all patients virtually first, regardless of their concerns, and then determine if the patient needed to be seen in person. As COVID-19 case counts declined, PCCs were left to navigate how they approached integration of virtual care into practice.125 Some guidance emerged to support PCCs, for example, to use virtual care to optimize chronic condition care.106,126 However, as we move toward COVID-19 recovery, further research and guidance is needed on the optimal implementation of virtual care to balance issues related to equity, efficiency, patient-centredness, safety, and appropriateness.
Interpretation
Across Ontario, PCCs have played an integral and multi-faceted role in Ontario’s pandemic response. PCCs took on new roles related to COVID-19 prevention, assessment, and management while also addressing non-COVID-19 primary care services. Early in the pandemic, they were asked to prioritize COVID-19-related tasks and defer non-essential care. As the pandemic continued, PCCs were asked to resume all previous important roles while supporting COVID-19 efforts. The PCC workforce has supported community and hospital-led initiatives; as the pandemic has continued, COVID-19-related work is increasingly being integrated into PCPs without additional supports or resources. PCPs with direct funding for interprofessional teams have inherently had more resources to support COVID-19 and non-COVID-19 prevention and care, from COVID@Home programs to maintenance of preventive care and chronic disease management—but these teams serve less than one-quarter of Ontario’s population.127,128 Substantial variation in both COVID-19 and non-COVID-19 care across the primary care sector highlights the need for regional primary care networks and data-driven responses to support best practice.
PCCs were engaged in COVID-19 assessment and testing efforts from the start, staffing assessment centres and doing testing outreach. However, multiple barriers prevented widespread assessment and testing within primary care offices during the early phases of the pandemic, including concerns for patient and staff safety, physical space constraints, workflow challenges, and in the first few months, availability of PPE.13
PCCs also provided wraparound services, remote monitoring, and treatment for people with COVID-19, as well as support for those with post COVID-19 condition. Programs such as COVID@Home have ensured rapid and equitable reach of COVID-19 care, and the successful rollout of Paxlovid through PCCs demonstrates the promise of implementing new clinical interventions by using existing communication and support pathways in primary care rather than building new infrastructure outside it.
PCCs not only administered COVD-19 vaccines but were trusted sources of information and outreach. Vaccination efforts initially drew PCCs away from their offices and towards mass vaccination sites, given challenges with supply chain, information technology, resource constraints, and financial structures that incentivized vaccine delivery outside of PCPs. Ontario has achieved a high two-dose vaccination rate, but booster doses and vaccination for children are lagging. PCCs deliver most routine immunizations, and lack of integration into this routine delivery channel may compromise ongoing COVID-19 vaccination uptake. The current suboptimal uptake is influenced by many factors, including public fatigue and lack of confidence among parents, but also significant challenges to integrating COVID-19 vaccination into the workflows of primary care.
Throughout the pandemic, PCCs across Ontario have led initiatives to close equity gaps in COVID-19 prevention and care. There was a historic mobilization of resources by community-based organizations in collaboration with PCCs from equity-deserving backgrounds, PHUs, and hospitals to support vaccination in marginalized communities. FNIM and Black PCCs and their allies formed new and innovative collaborations to address mistrust rooted in decades of unjust and unethical treatment of FNIM and Black people and communities in Canada. They ensured vaccines were easy to access by those who were most vulnerable to the impacts of COVID-19.
In the midst of these efforts, PCCs provided ongoing non-COVID-19 care addressing a range of patient needs from preventive services to care for chronic conditions and mental health and addictions, all while facing growing care demands due to delayed surgeries and services. Although some elements of care (such as immunization for infants) were maintained, other areas have shown significant care lags (such as cancer screening and chronic condition care). Reasons for care gaps are multifactorial and include directions from government to defer preventive care, reasonable deferral of care for more people with stable disease, patients themselves opting to delay seeking care, and potentially the accessibility of primary care physicians.
PCCs increased the use of virtual care while navigating issues of equitable access and while competing commercial ventures drew patients away from establishing an ongoing relationship with a primary care provider. With the use of virtual care, total visit volumes in primary care returned to pre-pandemic levels within six months of the pandemic star. Provider and patient satisfaction with virtual care is high, and recent data estimate that just under half of care is being delivered virtually. Most virtual care is delivered by phone, and more work is needed to understand how best to integrate other modalities, including asynchronous messaging and video. More evidence is also needed to guide and enhance the appropriateness, safety, and equity of virtual care. A very small proportion of PCCs shifted to a solely virtual model which likely reduced quality of care for conditions where in-person assessments were necessary.
PCCs play a unique role in the healthcare system, given the long-term relationships and trust built with patients over time, their role in care coordination, and their commitment to whole-person care. In the current phase of the pandemic, and looking ahead, the role of PCCs will be especially important given high levels of deferred care, long waits for specialty care and diagnostics, rising need for mental health and addictions care, persistent gaps in health equity, and the need for clear communication to the public about how best to access the system and what to expect. However, maintaining core primary care services while continuing to provide capacity to prevent, assess, and manage COVID-19 patients in the community will be increasingly challenging given fixed practice resources, suboptimal data and quality improvement infrastructure, and the limited number of PCPs supported with dedicated funding for dedicated teams. The challenge of supporting Ontarians with COVID-19 and non-COVID-19 care will be greatest for the hundreds of thousands of Ontarians who do not have a regular PCC or team and are therefore unable to benefit from primary care.
Methods Used for This Science Brief
The following methods were used in a single common strategy to construct all three parts of this Science Brief; subsequent to the writing of the first draft of the Brief; a decision was taken to divide the content into three parts.
We sought peer-reviewed literature as well as relevant pre-prints, academic presentations, reports, manuals, and other grey literature in addition to data from media scans and health system sources to construct the fullest possible picture of the impact of COVID-19 pandemic on the state of primary care in Ontario and Canada.
We searched Ovid MEDLINE and limited the search strategy to studies from January 1, 2019 to July 27, 2022, using the COVID-19 filter adapted for search strategies created by Library and Knowledge Services of the National Health Services, using the key terms: “general practitioners or physicians”, “primary care, patient care team or hospital rapid response team or nursing”, “community health services or community health nursing or home care services”, “teams or attachment or universal or empanelment”, “interdisciplinary or multidisciplinary or system or primary or policy or service or delivery”, “delivery of health care”, “Ontario and Canada”. A grey literature search of relevant reports, manuals and policy papers was also done focusing on Primary care and COVID-19 pandemic response, Pandemic Recovery, Integration of care, and Team-Based Care. The grey literature search was not limited to the Canadian context and yielded seven primary reports. At the request of the authors, the Ontario Medical Association library team provided a scan of media and grey literature using the team’s daily in-house environmental scanning product, “The Scan”, focusing on articles and other materials addressing the “state of primary care in Ontario during the pandemic” from 2021 to 2022.
Our initial search results yielded a total of 215 reports and papers, which were shared in a common folder for review and analysis by study lead authors and co-authors. These were reviewed, with lead authors for each section using those papers relevant to their portion of the Brief and reviewed several times to ensure inclusion of relevant evidence in each section of the Brief. Unpublished emerging data was sought out from relevant health system sources such as the Ministry of Health, Ontario Health, and the INSPIRE-Primary Health Care research team, with authors permission, to supplement published data.
Expert consensus was then sought on the basis of parts 1 and 2 to draw the “lessons learned” and recommendations outlined in part 3. This was an iterative process conducted with the six core co-authors representing family physician leaders and researchers affiliated with various academic institutions in Ontario. The process included virtual meetings, email communications and clarification of language. A simple analytical framework, Search, Appraisal, Synthesis and Analysis (SALSA) was employed, and a narrative summary was generated for each of three sections of this Brief.
Drafts of the Brief sections were shared with primary care stakeholders across the province, the country and internationally for feedback, including primary care clinicians and leaders associated with the Ontario Ministry of Health, Ontario Health, the Ontario Medical Association and Section of General and Family Practice, Alliance for Healthier Communities, Ontario College of Family Physicians, Association of Family Health Teams of Ontario, Seamless Care Optimizing the Patient Experience, Indigenous Primary Care Council and Black Physicians Association of Ontario. Based on the feedback, the project team and the COVID-19 Science Table provided additional comments and directions for policy recommendations.
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. https://doi.org/10.1111/j.1468-0009.2005.00409.x
- Organisation for Economic Cooperation and Development. Primary health care is associated with reduced use of costly hospital and emergency department inputs. https://doi.org/10.1787/9789264266414-en
- Starfield B. Is primary care essential? The Lancet. 1994;344(8930):1129-1133. https://doi.org/10.1016/S0140-6736(94)90634-3
- Bazemore A, Grunert T. Sailing the 7c’s: Starfield revisited as a foundation of family medicine residency redesign. Fam Med. 2021;53(7):506-515. https://doi.org/10.22454/FamMed.2021.383659
- Haldane V, Zhang Z, Abbas RF, et al. National primary care responses to COVID-19: A rapid review of the literature. BMJ Open. 2020;10(12):e041622. https://doi.org/10.1136/bmjopen-2020-041622
- How to improve primary healthcare to prepare for future pandemics. UNICEF: For Every Child. https://www.unicef.org/stories/how-to-improve-primary-healthcare-to-prepare-for-pandemics
- Scarpetta S, Pearson M, Colombo F. Strengthening the frontline: How primary health care helps health systems adapt during the COVID 19 pandemic. Organisation for Economic Co-operation and Development.Published February 2021. https://www.oecd.org/coronavirus/policy-responses/strengthening-the-frontline-how-primary-health-care-helps-health-systems-adapt-during-the-covid-19-pandemic-9a5ae6da/
- Li D, Howe AC, Astier-Peña MP. Primary health care response in the management of pandemics: Learnings from the COVID-19 pandemic. Aten Primaria. 2021;53:102226. https://doi.org/10.1016/j.aprim.2021.102226
- Vanstone M, Annis R, Backo-Shannon M. Primary Care 2025: Capitalizing on Rapid Change to Improve Ontario’s Primary Healthcare System. Department of Family Medicine, McMaster University; 2020. https://primaryon.ca/system/assets/assets/attachments/57/original/PrimaryCare2025.pdf
- Mathews M, Meredith L, Ryan D, et al. The roles of family physicians during a pandemic. Healthc Manage Forum. Published online July 17, 2022:8404704221112311. https://doi.org/10.1177/08404704221112311
- Wanat M, Hoste M, Gobat N, et al. Transformation of primary care during the COVID-19 pandemic: Experiences of healthcare professionals in eight European countries. Br J Gen Pract. 2021;71(709):e634-e642. https://doi.org/10.3399/BJGP.2020.1112
- Huston P, Campbell J, Russell G, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4). https://doi.org/10.3399/bjgpopen20X101128
- Unruh L, Allin S, Marchildon G, et al. A comparison of 2020 health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy. 2022;126(5):427-437. https://doi.org/10.1016/j.healthpol.2021.06.012
- Desborough J, Dykgraaf SH, Phillips C, et al. Lessons for the global primary care response to COVID-19: A rapid review of evidence from past epidemics. Fam Pract. 2021;38(6):811-825. https://doi.org/10.1093/fampra/cmaa142
- Hanson K, Brikci N, Erlangga D, et al. The Lancet Global Health Commission on financing primary health care: Putting people at the centre. Lancet Glob Health. 2022;10(5):e715-e772. https://doi.org/10.1016/S2214-109X(22)00005-5
- Pinto AD, Bloch G. Framework for building primary care capacity to address the social determinants of health. Can Fam Physician. 2017;63(11):e476-e482. https://www.cfp.ca/content/63/11/e476
- Ontario population projections. ontario.ca. Published 2022. http://www.ontario.ca/page/ontario-population-projections
- Stewart M, Ryan B. Ecology of health care in Canada. Can Fam Physician. 2015;61(5):449-453.https://www.cfp.ca/content/61/5/449
- White KL, Williams TF, Greenberg BG. The ecology of medical care. Bull N Y Acad Med. 1961;73(1):187-212. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2359390/
- OMA’s Ontario Health Teams White Paper: Early Learnings and Recommendations for the Evolution of OHTs.; 2020. https://www.oma.org/uploadedfiles/oma/media/public/ohts-white-paper.pdf
- Bhatti S, Rayner EC and J. A rapid primary healthcare response to COVID-19: An equity-based and systems - thinking approach to care ensuring that no one is left behind. Healthc Q. 2020;23(3). https://www.longwoods.com/content/26336/healthcare-quarterly/a-rapid-primary-healthcare-response-to-covid-19-an-equity-based-and-systems-thinking-approach-to
- Arsenault A, Barr J. Mobile medical team provides in-home care to help take pressure off hospitals. CBC. Published May 24, 2020. https://www.cbc.ca/news/health/virtual-triage-assessment-centre-renfrew-1.5579197
- Renfrew County Virtual Triage & Assessment Centre: “Clinical assessment centre” 24/7 support during the COVID-19 pandemic. https://rcvtac.ca/
- The EasT-FPN current initiatives. East Toronto Family Practice Network. https://eastfpn.org/current-initiatives
- Grant K. Toronto doctors take COVID-19 testing to the people in effort to contain pandemic. The Globe and Mail. Published June 5, 2020. https://www.theglobeandmail.com/canada/article-toronto-doctors-take-covid-19-testing-to-the-people-in-effort-to/
- OMA Analysis, OHIP Claims, Fiscal Years 2020 & 2021 (Unpublished Data). Ontario Medical Association; 2022.
- Kiran T, Green M, Wu F, Strauss R, Gozdyra P, Kopp A, Latifovic L, Frymore E, Glazier R. INSPIRE-Primary Health Care Program (Unpublished Data).; 2022.
- Primary care in the COVID era. Published 2022. https://maphealth.ca/primary-care-covid-era/
- Kiran T, Green ME, Strauss R, et al. Are primary care virtual visits associated with higher emergency department use? A cross-sectional analysis from Ontario, Canada. medRxiv. Published online September 9, 2022:2022.09.08.22278709. https://doi.org/10.1101/2022.09.08.22278709
- University of Toronto family medicine report - stronger together: Caring through crisis by department of Family and Community Medicine at the University of Toronto. Published December 8, 2021. https://issuu.com/dfcm/docs/uoftdfcm_fammedreport21_layout-4d
- Kiran T, Wang R, Handford C, et al. Keeping doors open: A cross-sectional survey of family physician practice patterns during COVID-19, needs, and intentions. medRxiv. Published online December 21, 2021:2021.12.20.21267918. https://doi.org/10.1101/2021.12.20.21267918
- Toronto Public Health to stop tracing close contacts of COVID cases in the community as infections soar. thestar.com. Published October 3, 2020. https://www.thestar.com/news/gta/2020/10/03/toronto-public-health-to-stop-tracing-close-contacts-of-covid-cases-in-the-community-as-infections-soar.html
- Public Health Agency of Canada. What we heard: Indigenous Peoples and COVID-19: Public Health Agency of Canada’s companion report. Published March 16, 2021. https://www.canada.ca/en/public-health/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19/indigenous-peoples-covid-19-report.html
- Contact tracing: Inspiring cultural safety in Indigenous communities. IPHCC learning portal. https://learningportal.iphcc.ca/cluevo/lms/my-learning-tree/contact-tracing-inspiring-cultural-safety-in-indigenous-communities/
- Cutting through the COVID confusion. Healthy Debate. Published January 31, 2022. https://healthydebate.ca/2022/01/topic/cutting-through-covid-confusion/
- “It’s unbelievable” Virtual reality allows Parry Sound seniors to explore the world. ParrySound.com. https://www.parrysound.com/community-story/10597546--it-s-unbelievable-virtual-reality-allows-parry-sound-seniors-to-explore-the-world/
- Ashcroft R, Donnelly C, Gill S, Dancey M, Lam S, Mehta AKG and K. The delivery of patient care in Ontario’s family health teams during the first wave of the COVID-19 pandemic. Healthc Policy. 2021;17(2). https://doi.org/10.12927/hcpol.2021.26656
- Bhatti P, Rayner J. Using trusted relationships and community-led approaches to promote COVID-19 vaccine confidence and uptake across Ontario. [Accepted for Publication].; 2022.
- Supporting Health in Communities during COVID-19: How Community Primary Healthcare Delivered Continuous Care and Advanced Health Equity through the Pandemic Crisis. Alliance for Healthier Communities; 2021. https://www.allianceon.org/sites/default/files/supporting_health_in_communities_through_covid_-_2021-12-08.docx.pdf
- COVID@Home for Primary Care: What Is It? Ontario Health. https://www.ontariofamilyphysicians.ca/tools-resources/covid-19-resources/covid-at-home-02sat.pdf
- Evaluation: the Ontario COVID@Home clinical pathway for primary care of acute covid illness: A report for the ontario ministry of health (Unpublished). Department of Family Medicine, McMaster University; 2022.
- Ontario COVID-19 Drugs and Biologics Clinical Practice Guidelines Working Group. Nirmatrelvir/Ritonavir (Paxlovid): What prescribers and pharmacists need to know. Ontario COVID-19 Science Advisory Table. https://doi.org/10.47326/ocsat.2022.03.55.1.0
- Past COVID-19 community of practice sessions. https://dfcm.utoronto.ca/past-covid-19-community-practice-sessions
- COVID-19: Clinical guidance for primary care providers. New guidance for the prescription of nirmatrelvir/ritonavir (Paxlovid). Centre for Effective Practice. https://tools.cep.health/tool/covid-19/#new-guidance-for-the-prescription-of-nirmatrelvir-ritonavir-paxlovidtm
- Digital health supports for COVID-19 therapeutics (i.e. Paxlovid). eHealth Centre of Excellence. https://ehealthce.ca/COVID-Therapeutics.htm
- Antiviral Treatment (Paxlovid) Is Available for Higher-Risk Individuals with COVID-19. Ontario Health; :2. https://www.ontariohealth.ca/sites/ontariohealth/files/2022-04/Paxlovid-PatientFactSheet.pdf
- Ballering AV, Zon SKR van, Hartman TC olde, Rosmalen JGM. Persistence of somatic symptoms after COVID-19 in the Netherlands: An observational cohort study. The Lancet. 2022;400(10350):452-461. https://doi.org/10.1016/S0140-6736(22)01214-4
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute COVID-19 in primary care. BMJ. 2020;370:m3026. https://doi.org/10.1136/bmj.m3026
- Post COVID-19 Condition: Guidance for Primary Care. Ontario Health; 2021:3. https://www.ontariohealth.ca/sites/ontariohealth/files/2021-12/PostCovidConditionsClinicalGuidance_EN.pdf
- Access to COVID-19 and post-COVID condition advice through eConsult. https://econsultontario.ca/wp-content/uploads/2022/01/2-eConsult-and-COVID-19.pdf
- Quinn KL, Katz GM, Bobos P, et al. Understanding the post COVID-19 condition (long COVID) in adults and the expected burden for Ontario. Sci Briefs Ont COVID-19 Sci Advis Table. 2022;3(65). https://doi.org/10.47326/ocsat.2022.03.65.1.0
- Kerr M, Ivers N, Khan S. The Impact of Primary Care Attachment Patterns on COVID-19 Vaccination Uptake in Ontario. [in Prep].; 2022.
- Jüni P, da Costa BR, Maltsev A, et al. Ontario Dashboard. Sci Briefs Ont COVID-19 Sci Advis Table. Published online February 18, 2022. https://doi.org/10.47326/ocsat.dashboard.2021.1.0
- Adverse Events Following Immunization (AEFIs) for COVID-19 in Ontario: December 13, 2020 to September 11, 2022. Public Health Ontario; 2022:31. https://www.publichealthontario.ca/-/media/documents/ncov/epi/covid-19-aefi-report.pdf?sc_lang=en
- Potter C. GPs delivered over two thirds of COVID vaccinations in phase 1 of the programme. Pulse Today. Published July 9, 2021. https://www.pulsetoday.co.uk/news/coronavirus/gps-delivered-over-two-thirds-of-covid-vaccinations-in-phase-1-of-the-programme/
- An Ontario company built Canada’s best vaccine booking system... for Nova Scotia. thestar.com. Published April 24, 2021. https://www.thestar.com/news/gta/2021/04/24/an-ontario-company-built-canadas-best-vaccine-booking-system-for-nova-scotia.html
- Public Health Agency of Canada. Demographics: COVID-19 vaccination coverage in Canada. Published January 15, 2021. https://health-infobase.canada.ca/covid-19/vaccination-coverage/
- Tang X, Gelband H, Nagelkerke N, et al. COVID-19 vaccination intention during early vaccine rollout in Canada: A nationwide online survey. Lancet Reg Health – Am. 2021;2. https://doi.org/10.1016/j.lana.2021.100055
- Goldenberg MJ. Vaccines, values and science. Can Med Assoc J. Published online April 2019. https://www.cmaj.ca/content/191/14/e397
- With vaccines coming, family doctors could jab millions more if fully involved. OCFP. Published March 23, 2021. https://www.ontariofamilyphysicians.ca/news-features/family-medicine-news/~203-With-Vaccines-Coming-Family-Doctors-Could-Jab-Millions-More-If-Fully-Involved?resourceID=171
- Greene J, Ramos C. A mixed methods examination of health care provider behaviors that build patients’ trust. Patient Educ Couns. 2021;104(5):1222-1228. https://doi.org/10.1016/j.pec.2020.09.003
- Ivers N, Kiran T. COVID-19 vaccination in Canada: An educational series for primary care professionals. Department of Family & Community Medicine. Published August 12, 2020. https://www.dfcm.utoronto.ca/covid19-vaccination-modules
- Category archives: COVID-19. Marathon Family Health Team. https://mfht.org/category/covid-19/
- Confused about COVID? Family doctors answer your questions. https://dfcm.utoronto.ca/confused-about-covid
- Accessing COVID-19 vaccination data. OntarioMD. https://www.ontariomd.ca/covid-19/accessing-vaccine-data
- Women’s College Hospital. Big data and little behaviours: Feedback and quality improvement supports to primary care to facilitate COVID-19 vaccine uptake. clinicaltrials.gov; 2022. https://clinicaltrials.gov/ct2/show/NCT05099497
- Allergy advice for COVID-19 vaccine is now available on the Ontario eConsult service. eConsult. Published February 2, 2021. https://econsultontario.ca/allergy-advice-for-covid-19-vaccine-is-now-available-on-the-ontario-econsult-service/
- Helping hands: U of T med students aid family doctors in fulfilling COVID vaccine needs. Published August 17, 2022. https://dfcm.utoronto.ca/news/helping-hands-u-t-med-students-aid-family-doctors-fulfilling-covid-vaccine-needs
- Community vaccination promotion - Ontario (CVP-ON). Alliance for Healthier Communities. https://www.allianceon.org/Community-Vaccination-Promotion-In-Ontario
- Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74(11):964-968. https://doi.org/10.1136/jech-2020-214401
- Wilkins CH, Friedman EC, Churchwell AL, et al. A systems approach to addressing COVID-19 health inequities. NEJM Catal. 2(1). https://doi.org/10.1056/CAT.20.0374
- Riou J, Panczak R, Althaus CL, et al. Socioeconomic position and the COVID-19 care cascade from testing to mortality in Switzerland: A population-based analysis. Lancet Public Health. 2021;6(9):e683-e691. https://doi.org/10.1016/S2468-2667(21)00160-2
- Green MA, García-Fiñana M, Barr B, et al. Evaluating social and spatial inequalities of large scale rapid lateral flow SARS-CoV-2 antigen testing in COVID-19 management: An observational study of Liverpool, UK (November 2020 to January 2021). Lancet Reg Health – Eur. 2021;6. https://doi.org/10.1016/j.lanepe.2021.100107
- Vandentorren S, Smaïli S, Chatignoux E, et al. The effect of social deprivation on the dynamic of SARS-CoV-2 infection in France: A population-based analysis. Lancet Public Health. 2022;7(3):e240-e249. https://doi.org/10.1016/S2468-2667(22)00007-X
- Public Health Agency of Canada. From risk to resilience: An equity approach to COVID-19.; 2020. https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/from-risk-resilience-equity-approach-covid-19/cpho-covid-report-eng.pdf
- Tracking COVID-19 through race-based data. Ontario Health; :25. https://www.ontariohealth.ca/sites/ontariohealth/files/2021-08/Tracking%20COVID%2019%20Through%20Race%20Based%20Data-EN.pdf
- Statistics Canada Government of Canada. Impacts of COVID-19 on immigrants and people designated as visible minorities. Published October 20, 2020. https://www150.statcan.gc.ca/n1/pub/11-631-x/2020004/s6-eng.htm
- City of Toronto. COVID-19: Ethno-racial identity & income. City of Toronto. Published June 1, 2021. https://www.toronto.ca/home/covid-19/covid-19-pandemic-data/covid-19-ethno-racial-group-income-infection-data/
- Shah BR, Slater M, Frymire E, et al. Use of the health care system by Ontario First Nations people with diabetes: A population-based study. Can Med Assoc Open Access J. 2020;8(2):E313-E318.https://doi.org/10.9778/cmajo.20200043
- Ravichandiran N, Mathews M, Ryan BL. Utilization of healthcare by immigrants in Canada: A cross-sectional analysis of the Canadian Community Health Survey. BMC Prim Care. 2022;23(1):69. https://doi.org/10.1186/s12875-022-01682-2
- Glazier RH, Gozdyra P, Kim M, et al. Geographic variation in primary care need, service use and providers in Ontario, 2015/16. ICES; :150. https://maphealth.ca/wp-content/uploads/2019/10/Full-Report-Geographic-Variation-in-Primary-Care-Need-Service-Use-and-Providers-in-Ontario-August-2018.pdf
- Mosby I, Swidrovich J. Medical experimentation and the roots of COVID-19 vaccine hesitancy among Indigenous Peoples in Canada. CMAJ. 2021;193(11):E381-E383. https://doi.org/10.1503/cmaj.210112
- Eissa A, Lofters A, Akor N, Prescod C, Nnorom O. Increasing SARS-CoV-2 vaccination rates among Black people in Canada. CMAJ. 2021;193(31):E1220-E1221. https://doi.org/10.1503/cmaj.210949
- Engaging indigenous communities: With COVID-19 vaccine implementation. IPHCC. https://iphcc.ca/wp-content/uploads/2022/08/Effective-Engagement-Toolkit.pdf
- Kennedy B. Indigenous people in Toronto have much higher rates of COVID hospitalization than general population, new data shows. Published 2021. https://www.thestar.com/news/gta/2021/04/25/indigenous-people-in-toronto-have-much-higher-rates-of-covid-hospitalization-than-general-population-new-data-shows.html
- Indigenous Services Canada. Operation Remote Immunity 3.0 wraps up after coordinating nearly 200 vaccine clinics in 29 remote and isolated communities. Published February 22, 2022. https://www.canada.ca/en/indigenous-services-canada/news/2022/02/operation-remote-immunity-30-wraps-up-after-coordinating-nearly-200-vaccine-clinics-in-29-remote-and-isolated-communities.html
- Rich culture and resilience: Reflections on Operation Remote Immunity. Research, Education, Faculty & Staff, Giving, Inclusion & Diversity. Published April 2021. https://temertymedicine.utoronto.ca/news/rich-culture-and-resilience-reflections-operation-remote-immunity
- Smylie J, McConkey S, Rachlis B, et al. Uncovering SARS-COV-2 vaccine uptake and COVID-19 impacts among First Nations, Inuit and Métis Peoples living in Toronto and London, Ontario. CMAJ. 2022;194(29):E1018-E1026. https://doi.org/10.1503/cmaj.212147
- COVID-19 vaccine willingness among Canadian population groups. Statistics Canada. Published March 26, 2021. Accessed June 12, 2021. https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00011-eng.htm
- Family doctors help lead black health vaccine initiative. University of Toronto: Temerty Faculty of Medicine. Published May 2021. https://temertymedicine.utoronto.ca/news/family-doctors-help-lead-black-health-vaccine-initiative
- COVID-19: Black health alliance. https://blackhealthalliance.ca/covid-19/
- Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193(6):E200-E210. https://doi.org/10.1503/cmaj.202303
- Bronskill SE, Maclagan LC, Maxwell CJ, et al. Trends in health service use for Canadian adults with dementia and parkinson disease during the first wave of the COVID-19 pandemic. JAMA Health Forum. 2022;3(1):e214599. https://doi.org/10.1001/jamahealthforum.2021.4599
- Tu K, Sarkadi Kristiansson R, Gronsbell J, et al. Changes in primary care visits arising from the COVID-19 pandemic: An international comparative study by the International Consortium of Primary Care Big Data Researchers (INTRePID). BMJ Open. 2022;12(5):e059130. https://doi.org/10.1136/bmjopen-2021-059130
- Agarwal P, Wang R, Meaney C, et al. Sociodemographic differences in patient experience with primary care during COVID-19: Results from a cross-sectional survey in Ontario, Canada. BMJ Open. 2022;12(5):e056868. https://doi.org/10.1136/bmjopen-2021-056868
- Kaplan D. COVID Recovery. COVID-19 Community of Practice for Ontario Family Physicians; 2022. https://dfcm.utoronto.ca/sites/default/files/inline-files/March%2025_%202022%20COVID-19%20CoP%20Slide_v3.pdf
- Balancing demands: Considerations for family physicians. Ontario College of Family Physicians; 2022. https://www.ontariofamilyphysicians.ca/tools-resources/covid-19-resources/clinical-care-office-readiness/covid-balancing-demands.pdf
- Lofters AK, Mark A, Taljaard M, Green ME, Glazier RH, Dahrouge S. Cancer screening inequities in a time of primary care reform: A population-based longitudinal study in Ontario, Canada. BMC Fam Pract. 2018;19(1):147. https://doi.org/10.1186/s12875-018-0827-1
- Kiran T, Glazier RH, Moineddin R, Gu S, Wilton AS, Paszat L. The impact of a population-based screening program on income- and immigration-related disparities in colorectal cancer screening. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2017;26(9):1401-1410. https://doi.org/10.1158/1055-9965.EPI-17-0301
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: Systematic review and meta-analysis. BMJ. 2020;371:m4087. https://doi.org/10.1136/bmj.m4087
- Lofters A, Green M, Kiran T, Wu F, Vahabi M, Kopp A, Frymire E, Glazier R. Unpublished Analysis of ICES Data from INSPIRE-PHC.; 2022.
- Cronin CJ, Evans WN. Excess mortality from COVID and non-COVID causes in minority populations. Proc Natl Acad Sci. 2021;118(39):e2101386118. https://doi.org/10.1073/pnas.2101386118
- Dey S, Davidson J. The determinants of non-COVID-19 excess deaths during the COVID-19 pandemic: A cross-country panel study. Stud Microecon. 2021;9(2):196-226. https://doi.org/10.1177/23210222211046412
- McGrail K. Excess mortality, COVID-19 and health care systems in Canada. CMAJ. 2022;194(21):E741-E745. https://doi.org/10.1503/cmaj.220337
- Valabhji J, Barron E, Gorton T, et al. Associations between reductions in routine care delivery and non-COVID-19-related mortality in people with diabetes in England during the COVID-19 pandemic: A population-based parallel cohort study. Lancet Diabetes Endocrinol. 2022;10(8):561-570. https://doi.org/10.1016/S2213-8587(22)00131-0
- Kiran T, Moonen G, Bhattacharyya OK, et al. Managing type 2 diabetes in primary care during COVID-19. Can Fam Physician. 2020;66(10):745-747. https://www.cfp.ca/content/66/10/745
- Basu S, Phillips RS. Primary care in the COVID-19 pandemic: Improving access to high-quality primary care, accelerating transitions to alternative forms of care delivery, and addressing health disparities.; 2021:319. https://www.milbank.org/wp-content/uploads/2021/04/Book_Primary_Care_During_COVID_ebook_4-27-21.pdf
- Jones A, Bronskill SE, Maclagan LC, et al. Examining the immediate and on-going changes in claims-based incidence of dementia associated with the COVID-19 pandemic (Under review with BMJ Open).; 2022.
- Statistics Canada Government of Canada. Survey on COVID-19 and mental health, February to May 2021. Published September 27, 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210927/dq210927a-eng.htm
- One year into pandemic, about one in five Canadians reporting high levels of mental distress. CAMH. Published 2021. https://www.camh.ca/en/camh-news-and-stories/one-in-five-canadians-reporting-high-levels-of-mental-distress
- Statistics Canada Government of Canada. Self-rated mental health decreases after another year of the COVID-19 pandemic. Published June 7, 2022. https://www150.statcan.gc.ca/n1/daily-quotidien/220607/dq220607e-eng.htm
- Statistics Canada Government of Canada. Alcohol and cannabis use during the pandemic: Canadian perspectives survey series 6. Published March 4, 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210304/dq210304a-eng.htm
- Briefing series on the role of psychology in health care: Primary care. APA Center for Psychology and Health; 2014. https://www.apa.org/health/briefs/primary-care.pdf
- Stephenson E, Butt DA, Gronsbell J, et al. Changes in the top 25 reasons for primary care visits during the COVID-19 pandemic in a high-COVID region of Canada. PLOS ONE. 2021;16(8):e0255992. https://doi.org/10.1371/journal.pone.0255992
- Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64(11):832-840. https://www.cfp.ca/content/64/11/832
- Mental health and addictions system performance in Ontario: 2021 scorecard. CHART PACK; 2021:160. https://www.ontariohealth.ca/sites/ontariohealth/files/2021-02/ChartPack.pdf
- Patient resources: Mental health and addictions. Ontario College of Family Physicians; 2021. https://www.ontariofamilyphysicians.ca/tools-resources/covid-19-resources/community-supports-special-populations/ocfp-mh-patient-resources.pdf
- Richards DA, Toop LJ, Epton MJ, et al. Home management of mild to moderately severe community-acquired pneumonia: A randomised controlled trial. Med J Aust. 2005;183(5):235-238. https://doi.org/10.5694/j.1326-5377.2005.tb07026.x
- Caplan GA, Sulaiman NS, Mangin DA, Aimonino Ricauda N, Wilson AD, Barclay L. A meta-analysis of “hospital in the home.” Med J Aust. 2012;197(9):512-519. https://doi.org/10.5694/mja12.10480
- Ashcroft R, Saluja K, Ryan B, et al. Recommendations for virtual care in primary care practices: A survey of patients across Ontario, Canada. Ann Fam Med. 2022;20(Supplement 1). https://doi.org/10.1370/afm.20.s1.2947
- Chan-Nguyen S, Ritsma B, Nguyen L, Srivastava S, Shukla G, Appireddy R. Virtual care access and health equity during the COVID-19 pandemic, a qualitative study of patients with chronic diseases from Canada. Digit Health. 2022;8:20552076221074490. https://doi.org/10.1177/20552076221074486
- Gignac D. 2021 national survey of Canadian physicians: Quantitative market research report. Canadian Medical Association; 2021:32. https://www.infoway-inforoute.ca/en/component/edocman/3935-2021-national-survey-of-canadian-physicians/view-document?Itemid=0
- Opinion: The dark side of Canada’s shift to corporate-driven health care. The Globe and Mail. Published April 30, 2021. https://www.theglobeandmail.com/opinion/article-the-dark-side-of-canadas-shift-to-corporate-driven-health-care/
- Lapointe-Shaw L, Salahub C, Bhatia RS, et al. Characteristics and healthcare use of patients attending virtual walk-in clinics: A cross-sectional analysis. medRxiv. Published online March 1, 2022:2022.02.28.22271640. https://doi.org/10.1101/2022.02.28.22271640
- Kiran T. From virtual-first to patient-directed: A new normal for primary care. CMAJ Blogs. Published July 21, 2021. https://cmajblogs.com/from-virtual-first-to-patient-directed-a-new-normal-for-primary-care/
- Virtual care: Chronic conditions. Centre for Effective Practice. https://cep.health/toolkit/virtual-care/
- Kiran T, Kopp A, Moineddin R, Glazier RH. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ. 2015;187(17):E494-E502.https://doi.org/10.1503/cmaj.150579
- Hutchison B, Glazier R. Ontario’s primary care reforms have transformed the local care landscape, but a plan is needed for ongoing improvement. Health Aff (Millwood). 2013;32(4):695-703. https://doi.org/10.1377/hlthaff.2012.1087
DaM, IB, AE, NI, TK, DM, SN, AP, KP wrote the first draft of the Science Brief with significant contributions from KB, AG, MG, LJ, DK, EM, DN, JR, FR. All authors revised the Science Brief critically for important intellectual content and approved the final version, and extensive work on references and figures was led by SB, AE, NSB and AP. International unpublished data were provided by MK and SH.
Robust external review was then conducted and feedback incorporation and further revision were led by TK (part 1), DM and KP (part 2), and NI (part 3), with support from SB, AE and DaM. All authors revised the parts of the Science Brief on which they are named for critically for important intellectual content.
The authors would like to thank Joanne Sung, Karen Lee, Pat Buczkowski, Mahta Norouzi, Roisin McElroy, Kieran Quinn and the University of Toronto library service for their contributions to the literature review, reference checking, assistance with figures, formatting, and copyediting of this Science Brief; Dan Warshafsky, Zahra Ismail, and the teams at INSPIRE-PHC, and the Ontario Hospital Association for the provision of data; the team at the Ontario Science Advisory Table secretariat as well as Karla Freeman and Rebecca Clark at the Department of Family Medicine McMaster University for their assistance and support with editing, formatting, and supporting review of the brief; Alisa Kim and the Department of Family and Community Medicine at the University of Toronto for support throughout the process.
Citation: Kiran T, Eissa A, Mangin D, et al. Brief on Primary Care Part 1: The roles of primary care clinicians and practices in the first two years of the COVID-19 pandemic in Ontario. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2022;3(67). https://doi.org/10.47326/ocsat.2022.03.67.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
Declaration of Interest: Imaan Bayoumi
Declaration of Interest: Susan Beazley
Declaration of Interest: Onil Bhattacharyya
Declaration of Interest: Beth Cowper-Fung
Declaration of Interest: Azza Eissa
Declaration of Interest: Richard H. Glazier
Declaration of Interest: Michael Green
Declaration of Interest: Allan K. Grill
Declaration of Interest: Sally Hall Dykgraaf
Declaration of Interest: Noah Ivers
Declaration of Interest: Liisa Jaakkimainen
Declaration of Interest: David M. Kaplan
Declaration of Interest: Michael R. Kidd
Declaration of Interest: Tara Kiran
Declaration of Interest: Rosemarie Lall
Declaration of Interest: Dee Mangin
Declaration of Interest: Claudia Mariano
Declaration of Interest: Danielle Martin
Declaration of Interest: Elizabeth Muggah
Declaration of Interest: Steve Nastos
Declaration of Interest: Sarah Newbery
Declaration of Interest: Dominik A. Nowak
Declaration of Interest: Onyenyechukwu Nnorom
Declaration of Interest: Kamila Premji
Declaration of Interest: Jennifer Rayner
