COVID-19 Vaccination for People with Disabilities
Authors:Sara Rotenberg, Matthew B. Downer, Hilary Brown, Jane Cooper, Sabrina Campanella, Yousef Safar, Gabrielle M. Katz, Sandi Bell, Wendy Porch, Fahad Razak, Paula A. Rochon, Michael Schull, Nathan M. Stall, Yona Lunsky on behalf of the Ontario COVID-19 Science Advisory Table
Key Message
Internationally, people with disabilities have been disproportionately impacted by COVID-19, accounting for nearly 60% of COVID-19 deaths in the UK and overall higher mortality rates based on social, clinical, and demographic factors.
Ontario has prioritized people with disabilities across the three phases of its COVID-19 vaccination program, but there is a difference between availability and accessibility of vaccination. Ontario’s 34 public health units are responsible for leading the local distribution and administration of COVID-19 vaccines, and their public facing websites serve as entry points for information on the accessibility of vaccination. On average, these websites contain information about 5 of 18 key accessibility features, across three domains: accessible communication, physical accessibility, and accessible social and sensory environments.
Ontario needs a multi-pronged strategy to reach all people with disabilities that includes improving information about communication accessibility, physical accessibility, and social and sensory environment accessibility throughout the COVID-19 vaccination journey. Ontario’s progress on vaccinating people with disabilities needs to also be measured through enhanced data monitoring efforts.
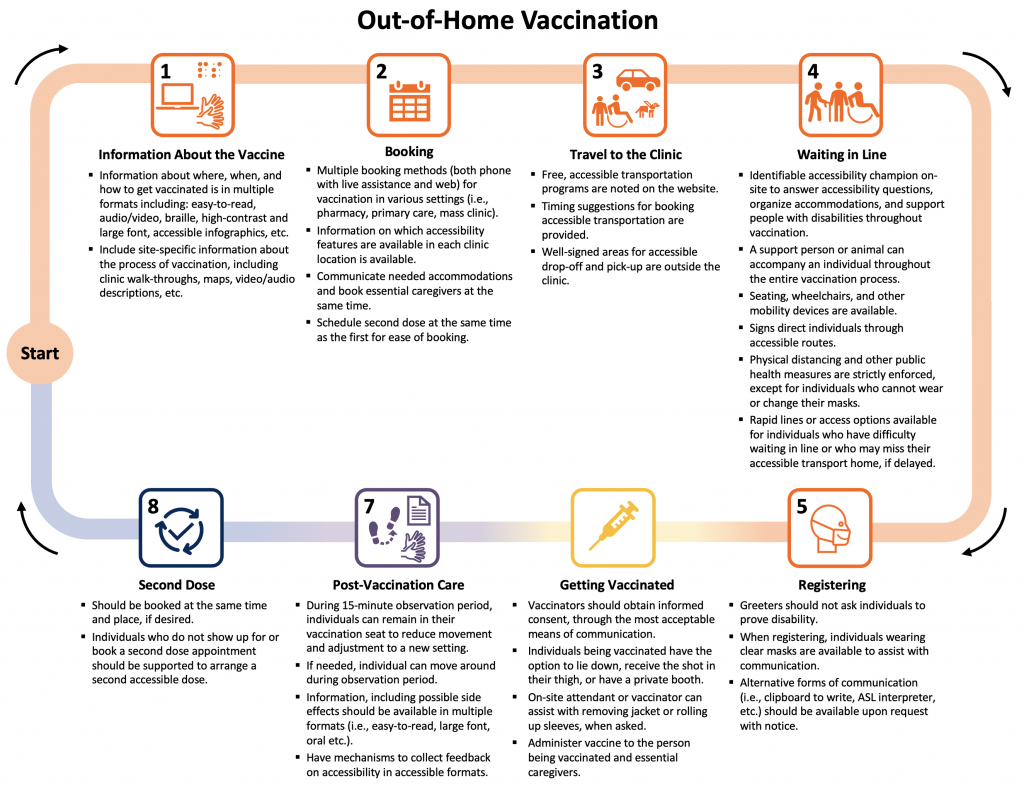
Presents the possible paths through out-of-home vaccination. Accessible information, booking processes, travel to the clinic, waiting in line, registration, vaccination, post-care, and second dose preparations are the critical steps where communications, physical and social and sensory environmental communications are important. For further details on important considerations within each of these steps, see Table 1. ASL, American Sign Language.
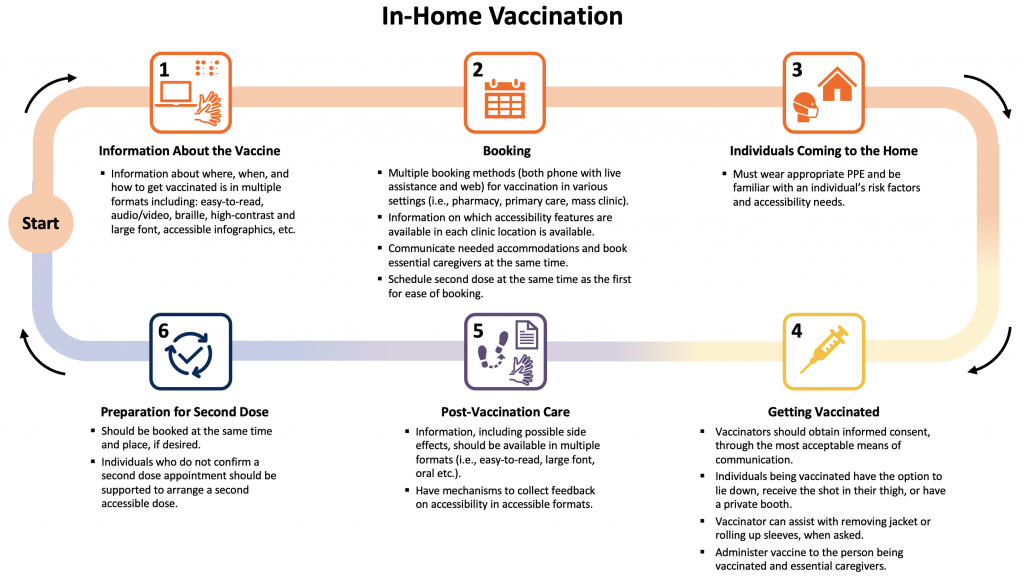
Presents the possible paths through in-home vaccination. The steps are similar on information, booking, post-care, and preparing for the second dose as for out-of-home vaccination, but vaccinators coming into the home should wear appropriate PPE and understand accessibility needs to support people with disabilities getting vaccinated in their home.
Summary
Background
One in five Ontarians has a disability — a physical, mental, intellectual, or sensory impairment — with the rate increasing to 40% of Ontarians over 65 years of age. A growing body of global evidence indicates people with disabilities have been disproportionately impacted by COVID-19. For instance, 59% of COVID-19 deaths in the UK occurred in people with disabilities, despite comprising 17% of the population.
While Canadian data are limited, there is a link between disability status and COVID-19 related hospitalizations and mortality. This has led Ontario and many other jurisdictions to prioritize specific groups of people with disabilities for COVID-19 vaccination. However, without supporting the accessibility and acceptability of vaccination, from providing information about vaccination the vaccination process to the actual vaccine administration, people with disabilities may face barriers in receiving their COVID-19 vaccine.
Questions
How have people with disabilities been impacted by COVID-19?
How have people with disabilities been prioritized in Ontario's COVID-19 vaccination plan, including for second dose interval exemptions?
What are the key considerations for making COVID-19 vaccinations accessible for people with disabilities?
What are the barriers to people with disabilities receiving the COVID-19 vaccine?
How can data monitoring on COVID-19 vaccination and disability inform accessibility initiatives?
Findings
International data suggest disproportionate impacts of COVID-19 on people with disabilities with a greater risk of morbidity and mortality as well as serious mental health and social impacts. Given these experiences, Ontario has prioritized many people with disabilities in the early phases of its vaccination rollout. Key considerations related to communication, the physical and the social and sensory environment can make vaccination more accessible for people with disabilities.
As a proxy for perceived and actual accessibility, a framework measuring 18 accessibility dimensions was developed and applied to review publicly available information on the websites of Ontario’s 34 public health units (PHUs) as of May 7, 2021. While this may not be fully representative of all accessibility initiatives, it simulates the user experience in trying to get information about available vaccination accommodations. Overall, the website review identified multiple potential barriers, as the median number of accessibility dimensions listed as available was 5 of 18 (inter-quartile range (IQR) 4-6), or 28% of the identified dimensions. Only five of the PHUs had more than 50% of the identified dimensions, while nine of the PHUs had less than 25% of the identified dimensions publicly available online. In addition to having some of these accessibility features within mass vaccination sites, some PHUs have also developed more specialized clinics focused on vaccinating people with disabilities and have offered mobile clinics to certain individuals.
Ontario has yet to track and report publicly on COVID-19 vaccination rates among all people with disabilities. Using people with intellectual and developmental disabilities—one of the high-risk subgroups prioritized in Phase 2—as an example, recent data from ICES demonstrate the feasibility and value of monitoring vaccination rates.
Interpretation
Making Ontario’s COVID-19 vaccination sites more accessible should build upon existing initiatives to improve communication-related, physical, and social and sensory accessibility at each stage of the vaccination process for all types of clinics. It is important to include all accessibility information in multiple formats on PHU websites to reduce barriers to vaccination, from booking to attending the vaccination clinics. Although accommodations may be available upon request, by phone or at specific clinics, if such information is difficult to access, this may prevent individuals with disabilities from pursuing vaccination. Accommodation request forms and other navigational supports at the time of booking and ‘accessibility champions’ on-site for every location can support people with disabilities in getting vaccinated.
PHUs can continue to provide and expand opportunities for acceptable and accessible care for people with disabilities at existing clinical vaccination sites, as well as through implementing more targeted approaches to reach people with disabilities, such as mobile in-home vaccination and specialized clinics. Collecting and publicly reporting data on vaccinations for people with disabilities can inform ongoing accessibility efforts.
Background
People with disabilities make up an estimated 22% of Ontarians.1 In Canada, the term ‘people with disabilities’ describes individuals who have long-term impairments that are physical, mental, intellectual, or sensory in nature and who face barriers to full and equal participation in society.2 Accessibility considerations address certain barriers to participation. While accessibility is often thought of in terms of physical accessibility (i.e., wheelchair accessibility, step-free access, etc.), it also encompasses communication and social and sensory environment-based accessibility. Many accommodations are simple, low- or no-cost, easy to implement and consistent with the requirements in the Accessible Canada Act, 2019; Canada Health Act, 1984; and Accessibility for Ontarians with Disabilities Act, 2005.
People with disabilities have been disproportionately impacted by the COVID-19 pandemic and are at a higher risk of contracting SARS-CoV-2. Several factors increase the risk of contracting SARS-CoV-2 for people with disabilities, including in-person care requirements, living in congregate settings including group and long-term care (LTC) homes, inaccessible public health messaging, and difficulty following some public health measures, among other factors. Furthermore, people with disabilities have higher rates of several chronic health conditions that are associated with COVID-19 outcomes such as hospitalization and death. These conditions can be associated with an individual’s disability but can also be the result of or exacerbated by poor access to health care.
While many provinces, including Ontario, have prioritized people with disabilities and those living in congregate settings for early COVID-19 vaccination, there is a difference between availability and accessibility of vaccines. Simply being eligible is not sufficient to ensure access to vaccines for people with disabilities, making it critical to address accessibility across the COVID-19 vaccination journey. Ultimately, many of these accessibility features will improve the vaccination experience for everyone — particularly having clear communication, easy to use resources and booking, and a more sensory friendly and physically accessible environment — making it important to implement universal accessibility into Ontario’s vaccination roll-out.
Questions
How have people with disabilities been impacted by COVID-19?
How have people with disabilities been prioritized in Ontario's COVID-19 vaccination plan, including for second dose interval exemptions?
What are the key considerations for making COVID-19 vaccinations accessible for people with disabilities?
What are the barriers to people with disabilities receiving the COVID-19 vaccine?
How can data monitoring on COVID-19 vaccination and disability inform accessibility initiatives?
Findings
Evidence on COVID-19 and Disability
International data illustrate the disproportionate impact COVID-19 has had on people with disabilities. Data from the UK demonstrate that 59% of COVID-19 deaths have been among people with disabilities.6 After adjusting for age, socio-demographic, and other risk-factors, in the pandemic’s first wave, people with disabilities, as measured by census data, were found to have mortality rates 2.4 and 2.0 times higher for women and men, respectively, regardless of disability type. 6,7
Furthermore, mortality rates are higher for people with certain specific disabilities. For example, a US study showed that intellectual disability is the strongest predictor for COVID-19 mortality after age,5 and other studies have estimated the mortality for people with Down syndrome is five to ten times that of the general population.6,7 In New York, people with schizophrenia spectrum disorder were found to have a death rate 2.67 times higher than others in the general population. In addition, certain conditions predispose individuals with disabilities to adverse outcomes of COVID-19, such as neuromuscular conditions that impact breathing, but limited data are available to assess the full impact and outcomes of these individuals.8 For example, people with multiple sclerosis who were non-ambulatory were 2.8 times more likely to be hospitalized,9 3.5 times more likely to require ICU admission/ventilation, and 25 times more likely to die from COVID-19. Data from Spain demonstrate that individuals with chronic neurological conditions were more likely to go to the emergency department earlier (average of 1.4 days) for milder symptoms and nonetheless experienced higher in-hospital mortality.10
Age is a well-established risk factor for COVID-19 mortality. Older adults with disabilities are more likely to die than younger adults with disabilities if they contract COVID-19. However, there is an increased risk of mortality in younger age groups of people with disabilities than younger people in the general population.3,11 People with disabilities also often have poorer social determinants of health, which impacts their susceptibility to SARS-CoV-2 infection and risk of COVID-19 mortality. For example, place of residence has significant impacts on COVID-19 mortality. In addition to challenges experienced by those living in poverty in close quarters, UK and US studies have highlighted that one of the strongest predictors of COVID-19 mortality for people with intellectual or developmental disabilities is living in a congregate setting.3,12,13
While published data have focused on people with developmental disabilities, many people with disabilities live in congregate settings or receive in-home support through community-based care. Ontario has prioritized congregate settings for people with disabilities such as LTC homes – where 6% of residents are younger adults with disabilities – for early COVID-19 vaccination in December 2020 and January 2021.14 In contrast to LTC homes, vaccinations in group homes and other supported residential settings only began during Phase 2 (March to May 2021); most, if not all of these settings have only been partially vaccinated, despite their high-risk populations and congregate nature.
Finally, people with disabilities have higher rates of a number of chronic health conditions that may be associated with one’s disability and may require home and community care supports. Many people with disabilities who live in the community have an increased risk of contracting SARS-CoV-2 because of in-person care requirements, such as personal care attendants who also serve multiple clients or unpaid family caregivers. Multimorbidity and comorbidities further increase the risk of COVID-19 incidence and mortality among people with disabilities. Health care access, especially during the pandemic, is more difficult for people with disabilities who are also racialized, newcomers, or living in poverty. Together, these demographic, social, and clinical risk factors may contribute to these disproportionate COVID-19 mortality trends for people with disabilities.
Importantly, the COVID-19 pandemic has also had a social impact on people with disabilities. For instance, poverty is more common for people with disabilities,15 with an estimated 58% of people with disabilities currently unemployed. During the pandemic, approximately 44% of employed Canadians with disabilities have had their hours reduced, have been laid off, or have been furloughed and remained ineligible for income support.16 In addition, people with disabilities faced barriers to accessing social support and other necessary care, as well as significant adverse outcomes of prolonged isolation.
A recent Canadian survey found that, because of the pandemic, people with disabilities’ unmet needs for social and non-COVID-19 related health services increased, particularly in the areas of home care; general, specialized, and mental health care; transportation; internet and technology; and equipment and medical supplies.16 While it is too soon to measure the long-term impacts of the loss of these services, it is likely that people with disabilities will be negatively impacted by functional, health, wellbeing, and learning losses for many years to come.17
Vaccination Accessibility in Ontario
People with disabilities fall into all three categories of Ontario’s COVID-19 vaccine prioritization framework. People with disabilities living in LTC homes, Indigenous Ontarians with disabilities, and adults with disabilities receiving chronic home care were eligible to be vaccinated in Phase 1, though individuals who stopped chronic home care to reduce the risk of infection were no longer eligible for Phase 1, even if vaccination would allow them to restart these critical services. People with disabilities in congregate settings or hot spot communities, and those with the highest-, high-, and at-risk conditions and their caregivers were included in Phase 2. Within these Phase 2 conditions, some specific disabilities, including ‘neurological diseases that impact breathing (i.e., multiple sclerosis, muscular dystrophy, etc.)’, “intellectual or developmental disabilities (i.e., Down syndrome)”, and “other disabilities requiring direct support care in the community”, were explicitly named. Other people with disabilities who do not fall into these categories should receive their vaccine in Phase 3, alongside the general population, unless they live in one of Ontario’s 114 ‘hot spot’ areas.
Although the province develops the provincial prioritization strategy, each PHU is responsible for determining community needs, and for leading the local distribution and administration of COVID-19 vaccines.18
Given that some people with disabilities are receiving their first vaccine doses alongside the general population, we identified key accessibility considerations to make vaccinations accessible to all people with disabilities. The considerations listed are consistent with Provincial Health Care Standards currently under public review. Many of these features are low- or no-cost and would also benefit people without disabilities. These include accessibility in the communications, physical, and social and sensory environment domains throughout each step involved in a vaccination program (Table 1).
| Phase | Communication | Physical | Social and sensory environment |
| Information about the vaccine, decision to get vaccinated, and booking process | Plain language and easy-to-read translation about when to get vaccinated, how vaccines work, how to get vaccinated, how to understand media about rare vaccination side effects, and the vaccination journey. Multiple, accessible formats of information, advertisements, and booking modalities (including information in multiple languages, plain text, pictorial representation, and text-to-speech compatible). Provide videos, pictures, site maps, and written easy-to-read documents to guide the vaccination journey, especially if people cannot preview the site ahead of time. |
Accessible booking website (i.e., screen readable, keyboard input, alternative text, no flashing components, etc.). | Web, phone, text, and primary care physician-based alternatives for booking vaccination and/or information about vaccination. |
| Eligibility/burden of proof | Information on required documents or processes for vaccination should be available online, if absolutely necessary. | Allow for paper or electronic documentation, if absolutely necessary. | Service providers do not ask for proof of disability. |
| Accessible line, approach, and entrance to vaccination center | Clear, large high-contrast signage indicating location of vaccination centre, line start/end, directional traffic, protocols, required questions, etc. International Symbol of Accessibility at accessible entrance. Clipboards to allow for written communication, clear masks, and sign language interpreters to communicate with people who are d/Deaf or hard of hearing. Any critical written communication should be available in braille cards or read to individuals who cannot read. |
Accessible entrance (wide doorway, low-force or automatic doors, ramp, no steps, etc.). Signage indicating accessibility and how to request accommodations. Nearby accessible parking and transportation stops. Accessible waiting areas with chairs for those unable to stand in long lines. Option to be vaccinated in a car for drive-through sites. Availability of wheelchairs on site to be used if needed, and cleaned between uses. Adequate spacing and strict public health measures to reduce exposure. Tactile paving to guide people with visual disabilities. Space/seat for support person and resting area for support animal with water bowls available. Accessible washrooms should be available. |
Provide a number to call/text before arrival to get support, accommodations, or immediate service on arrival (i.e., mask wearing exemption, wheelchair assistance, etc.). Have greeters present to assist patients with visual, physical, or cognitive disabilities. Ensure public health measures are strictly adhered to or enhance at certain locations for safety of higher-risk individuals. Provide a scent-free environment. Allow a support person to accompany people into the vaccination site (i.e., sign language interpreter, family member, PSW, etc.). Allow service/support animals to accompany individual |
| Vaccination experience | Ensure informed consent is obtained and the vaccination process is explained in clear, plain language. Clipboards, clear masks, and sign language interpreters to communicate with d/Deaf or hard of hearing patients. |
Option to lie-down for vaccination. Option to receive vaccine in the thigh (anterolateral thigh is authorized as a secondary injection site). Allow caregiver or support person to sit beside the individual. |
Provide safe environment for individuals who have difficulty wearing face masks. Separate table at each site that can accommodate individuals with disabilities (i.e., extra time, caregiver support, etc.). Ensure that a quiet, reduced sensory environment is available. Provide a rapid line or expedited service for people with disabilities who have difficulty waiting, being in a sensory environment, or have scheduled accessible transportation. |
| Waiting period | Bulleted, large-print handouts and alternative formats are available for key information. Plain language and easy-to-read translation about post-vaccination protocols and monitoring side effects. Provide risk communication about any side effects. |
Allow caregiver or support person to sit beside the individual. Have non-seated spaces for wheelchair users and clear pathways in between areas for people with visual impairments. Ensure waiting area is not a far walk from the vaccination site or provide the option of staying in-place, instead of moving from station to station. Provide a space to move during waiting period if staying in one place is hard. |
Provide opportunities to ask questions or discuss concerns about post-vaccine side effects. Provide a safe space within the setting if the sensory or physical environment is overwhelming or the individual is stressed and needs space to decompress. |
| Follow-up information and second appointment | Accessible and easy-to-read follow-up information with instructions for second dose of a two-dose vaccine booking or changes to booking (i.e., timing, location, etc.) communication. Individuals who do not show up for/book a second dose of a two-dose vaccine should be supported to arrange a second accessible dose. |
Endeavour to keep first and second doses of a two-dose vaccine at the same location and time. Allow people with disabilities to provide feedback on accessibility in accessible formats. |
Key accessibility considerations through each phase of the vaccination process. This table was adapted from McKee et al.19 PSW, personal support worker.
Eighteen accessibility dimensions that could be monitored through reviewing publicly available website information across three accessibility categories were examined on PHU websites:
- Communication: accessible website; multiple booking options; phone number available; sign language interpretation; information about requirements to move between stations at the vaccination centre; second appointment provided during first appointment.
- Physical Accessibility: ability to book appointments for pop-up clinics; private booths available; accessible entrance at site; wheelchair available on site; accessible post-vaccination waiting area, drive-through available; mobile in-home vaccination offered.
- Social/Sensory Environment: ability to bring a care partner; specialized clinic or hours for people with disabilities; no requirement/burden to offer proof of disability; ability to move around while waiting during the observation period; face mask exemption policy in place.
These dimensions were chosen as they were considered both feasible to assess online and captured important accessibility considerations for potential users seeking vaccination through PHU websites. They were also consistent with Ontario Health Care Accessibility Standards initial recommendations recently made available for public comment. No further research, such as individual site visits, phone calls, interviews with PHUs were conducted in order to ascertain the amount of accessibility information provided to a potential user seeking vaccination information. While this simulates the user’s experience, it does not capture additional accessibility information that may be available via phone call or visit to a specific vaccination site.
The breakdown of the accessibility information provided by Ontario PHU websites are detailed in Tables 2 to 4. Overall, the proportion of PHUs that provided various accessibility related information on their websites varied widely based on the specific accessibility dimension in question.
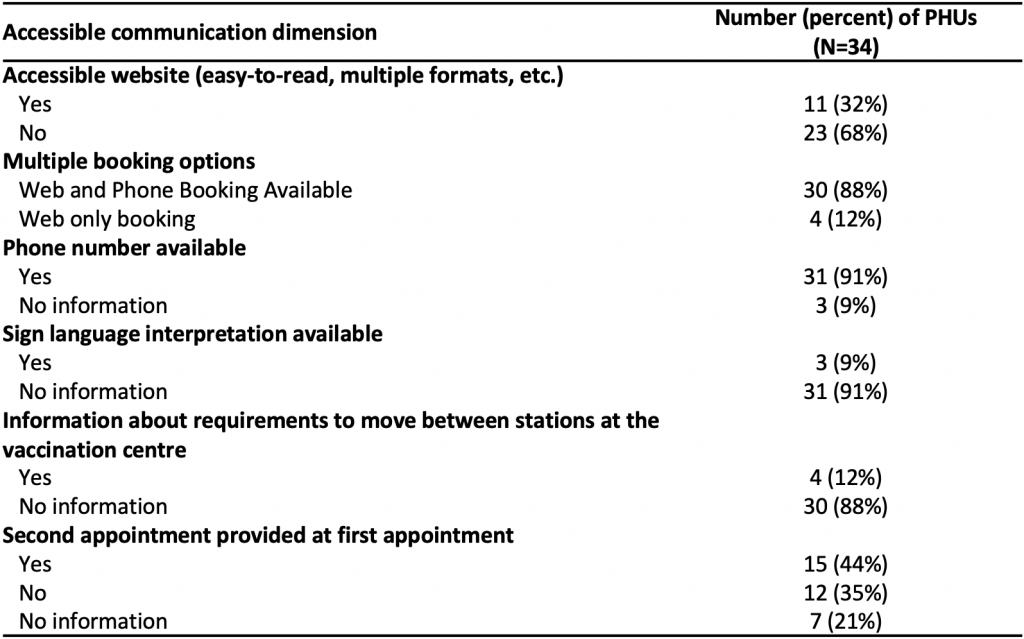
Table reporting the communications accessibility features publicly available on Ontario’s 34 PHU websites. Coding is based on information publicly available PHU websites, as of May 7, 2021 (see methods section below). However, this may not sufficiently capture the full degree of accessibility or inaccessibility of a vaccination site. In addition, several locations noted that additional needs could be met to accommodate people with disabilities, but where the measures were not clear or publicly available online, were not included in this analysis. PHU, public health unit.
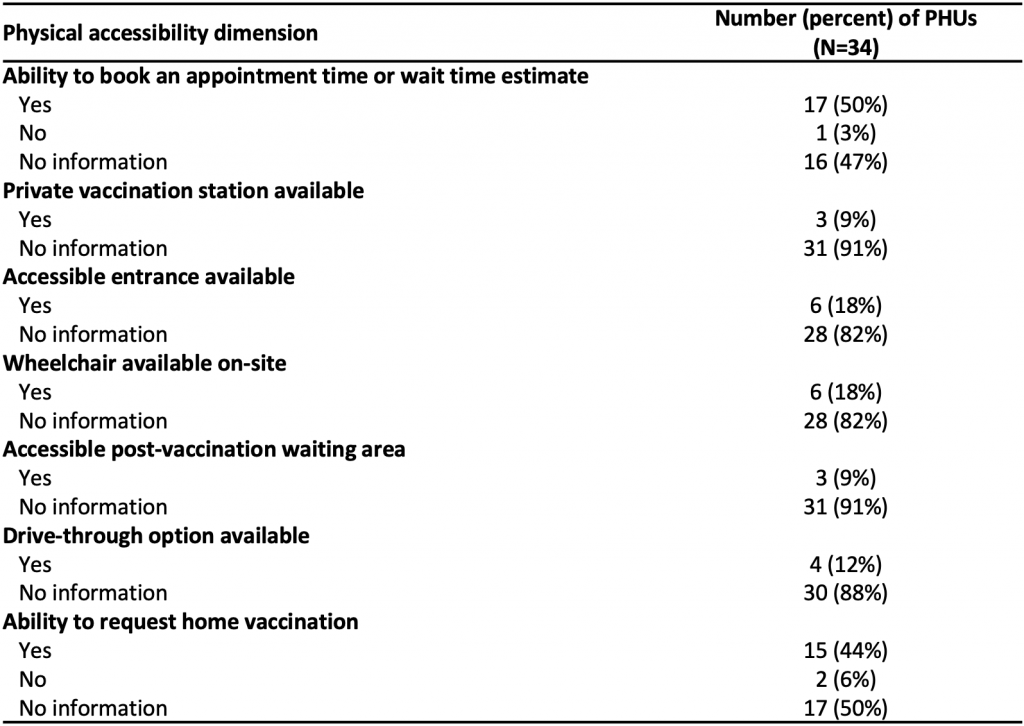
Table reporting the communications accessibility features available on Ontario’s 34 PHU websites. Coding is based on information publicly available on PHU websites, as of May 7, 2021 (see methods section below). However, this may not sufficiently capture the full degree of accessibility or inaccessibility of a vaccination site. In addition, several locations noted that additional needs could be met to accommodate people with disabilities, but where the measures were not clear or publicly available online, were not included in this analysis. PHU, public health unit.
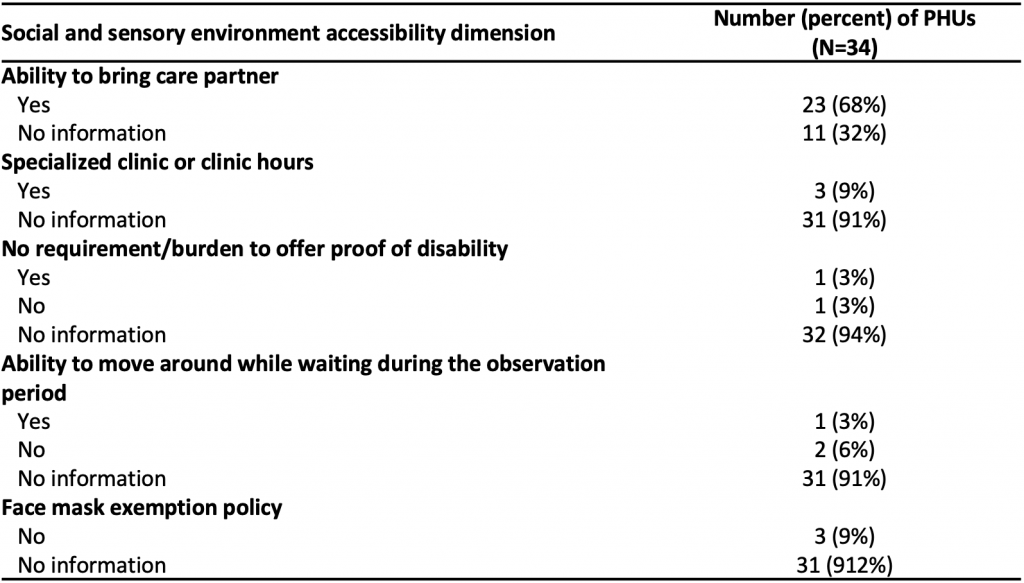
Table reporting the communications accessibility features available on Ontario’s 34 PHU websites. Coding is based on information publicly available PHU websites, as of May 7, 2021 (see methods section below). However, this may not sufficiently capture the full degree of accessibility or inaccessibility of a vaccination site. In addition, several locations noted that additional needs could be met to accommodate people with disabilities, but where the measures were not clear or publicly available online, were not included in this analysis. PHU, public health unit.
Accessibility information provided by specific Ontario PHUs are detailed in Figure 3. Accessibility information provided on the respective websites varied widely.
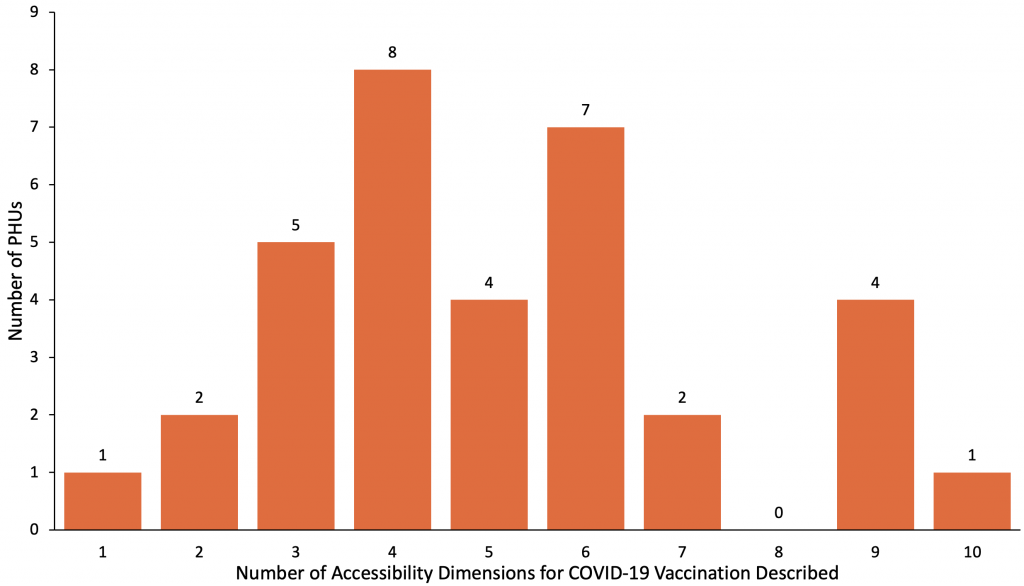
The number of accessibility dimensions described on each PHU website ranged from 1 to 10, out of the 18 key dimensions measured. The median was 5 (IQR 4-6). PHU, public health unit. IQR, inter-quartile range.
Communication Accessibility
Communication is a central tenet of the COVID-19 vaccination program – from information about vaccination benefits and risks, to eligibility, booking, and information regarding potential side effects.20 Any websites with information about the vaccine at both the provincial and PHU levels needs to be accessible and comply with the AODA, 2005. Presenting public health messaging in easy-to-read formats--using pictures, text, and audio formats--will support access to information. In particular, providing a guided tour of the process through captioned videos, words, and pictures can help ease anxiety about going into an unfamiliar place or process for many people with disabilities.
Accessible communication is one of the areas where Ontario’s vaccination program has been lacking, as only 32% of PHUs had some form of accessible format available on their websites (i.e., easy-to-read information about vaccines, walking tours/pictures of the process, etc.) and only 9% had noted sign language interpretation was available. Moreover, information on eligibility, and booking processes has evolved over time. Providing regularly updated information available in accessible formats (i.e., easy-to read, sign language interpretation, text, and audio, etc.) will be helpful for all Ontarians, particularly for people with disabilities.
Communication needs to outline various vaccine side effects clearly, the risk of side effects, how to monitor for side effects, and when one should seek care for specific symptoms in multiple formats. Furthermore, messaging and communication must include some guidance on when the vaccine will confer protection after vaccination, and how to stay safe after the first dose. This is particularly salient for people whose disabilities are associated with impaired immune function, such as Down syndrome, as well as people with disabilities that are traditionally excluded from clinical trials and/or for whom there are insufficient data on immune response or effectiveness of COVID-19 vaccines.21,22 Providing clear, risk-based guidance in accessible formats can help people with disabilities safely navigate the interval between doses.
Accessibility Considerations for Mass Vaccination Clinics and Community Pop-up Clinics
Booking is a critical barrier to accessing vaccination. While most PHUs had web and phone-based booking (88%) or phone numbers available (91%), a few relied exclusively on the provincial website, which can be inaccessible to people with literacy issues and screen reader users. Phone attendants may not be familiar with the accessibility of each PHU or vaccination location, or the website itself may be Web Content Accessibility Guidelines (WCAG) inaccessible,23 meaning it is unusable to people with visual impairments or those who use screen readers or other adaptive technology. Websites had a median of two total WCAG accessibility score errors (IQR 0-6) and one contrast error (IQR 0-10), as measured through the WAVE web accessibility evaluation tool. If websites are the only way to find phone numbers or are the only way someone can book a vaccination appointment in a PHU, these errors will inhibit access for some people with disabilities. Importantly, there is no option at the booking stage to indicate needed accommodations on the provincial site or most PHU sites and no standard mechanism for someone to assist in ensuring that these accommodations can be provided prior to the appointment or a helpline for accessibility issues.
Some people with disabilities require someone to support them leading up to and during the vaccination process, and two-thirds of PHUs explicitly permitted care partners. In contrast, information about which physical, sensory and social accommodations were available at clinics was frequently missing and what was listed was limited. This can result in confusion and uncertainty and additional barriers for people with disabilities in accessing vaccinations. In line with ensuring clear communication about mass immunization clinics, websites should clearly state not only which accessibility accommodations are available but also indicate which are unavailable and provide the registrant with a phone or web-based opportunity to discuss alternative accommodations. For example, few PHUs mentioned whether or not they had face mask exemption policies (91% had no information), and the ones that did explicitly stated there were no exemptions to the face masks policy (9%), which can be inaccessible for some people with disabilities unable to wear, change, or require assistance when putting on face masks. Few PHU’s (9%) listed they had private vaccination stations for those with needle phobias or sensory impairments, while the remainder had no information (91%). Similarly, 12% described that movement between stations was required as part of the vaccination process, while the majority had no information (88%). Several mass clinics have been set up for individuals to stay in the same place throughout the vaccination process; such features should be noted online so that individuals know where these accessibility features are available.24 These are important components of the vaccine experience that, if unlisted and/or unavailable, may deter an individual from seeking vaccination in that environment. Importantly, there needs to be a mechanism, such as accommodation request forms within each vaccination website and phone number, to share information about accommodations so the clinic will be alerted to these needs prior to the appointment and can respond with additional information if required. Someone physically present at the clinic should also be able to follow up on accommodation requests.
Pop-up locations have been an effective strategy to reach individuals in ‘hot spot’ areas of high COVID-19 incidence and transmission, and have generally used a walk-in model.25 Data from Toronto show that allowing walk-in appointments through pop-up vaccination clinics, in some areas, have helped to reduce race-based disparities in COVID-19 vaccine access.26,27 However, while these have improved access for residents of high SARS-CoV-2 risk areas, many images of these locations reveal opportunities to improve accessibility, particularly for at-risk people with disabilities. For example, long wait times, no seating, sensory-heavy environments including ambient noise and music, and limited communication support present substantial barriers. In addition, short-notice pop-up clinics may not allow people with disabilities sufficient time to organize transportation, attendants/in-person support, or other accommodations. Rapid lines or specialized hours/options for people with disabilities who cannot wait in line can be implemented alongside a walk-in model; advertising a clinic phone number to call ahead or ask about accommodations would also be helpful. Information about accessible options can also be communicated through these local community and hospital-based partners, to assist communities in reaching those with disabilities. Otherwise, people may not realize that the pop-up clinic can offer accommodations to meet their needs.
All clinics, regardless of their format (i.e., mass, specialized, pop-up) should have a designated contact or ‘accessibility champion’ to answer questions about accessibility (at booking, prior to the appointment, and onsite), to implement accommodations, and support people with disabilities in being vaccinated.
Targeted Approaches
Specialized Clinics
Specialized clinics serving the accessibility needs of specific populations have been a useful tool around the world, and were listed as options for individuals on three PHU websites (9%). There are several examples of innovations across the province in this regard, although the information about accessible efforts may not have been highlighted on the PHU websites. Some examples of recently publicized clinics include: designated vaccination dates across two sites and an in-car option in York Region for 2000 people with developmental disabilities and their caregivers;28 the Centre for Addiction and Mental Health (CAMH) in Toronto prioritized vaccinating individuals with mental illness and developed a specialized clinic for youth and adults with developmental disabilities;29 and a special low-sensory pop-up clinic for adults with disabilities and caregivers in the Region of Waterloo.30 The City of Toronto’s Accessibility Task Force on COVID-19 Vaccines also partnered with Toronto Public Health to organize a cross-disability accessible COVID-19 vaccination clinic, which offered supports such as sighted guides, attendant care, sign language interpretation and mobility support.31 For this clinic, people could register in advance and list accommodation requests, which were followed-up on as required. Specialized clinics have also been developed for children with disabilities and medical complexities who are now eligible for vaccination.32 Community outreach and lead time is important for these specialized clinics so that clinics and community partners can assist with registration and give people extra time to prepare, and arrange necessary supports. Where designated clinics are not feasible or there is insufficient demand, PHUs can work with people with disabilities and community partners to find accessible solutions. Increasing the availability of specialized clinics, as well as having appointments available in more familiar settings, such as primary health clinics or pharmacies can reduce barriers or anxiety over new, large, sensory-heavy, and unfamiliar environments.33
Mobile and In-Home Clinics
As previous Science Briefs have shown,34,35 mobile clinics can be effective in reaching people who may face barriers accessing traditional vaccination sites. Mobile and in-home clinics were noted as being available in 15 (44.1%) PHUs, though many said they would start these in the near future. These clinics may be especially important in remote areas without comprehensive accessible transit systems or where vaccines are only available at mass clinics. It is important that these options are available to people who may not be considered ‘homebound’ (i.e., cannot leave their homes in any circumstances), but would find the process of out-of-home vaccination inaccessible even with accommodations and would otherwise not get vaccinated, despite their risk. In addition, mobile approaches are critical to reach those in congregate care, but communication or a schedule should be provided to residents,36 families, and caregivers so that there is adequate support and planning to ensure the vaccination experience is comfortable and accessible. There are currently many individuals waiting for mobile in-home vaccination, so increasing mobile vaccine resources is critical.
Monitoring of Vaccinations for People with Disabilities in Ontario
Disability specific algorithms can be created using existing administrative health data to monitor and publicly report on vaccination rates for people with disabilities. These algorithms use diagnostic codes in outpatient, emergency, and inpatient databases to indicate the presence of disability.37–39 Although currently available algorithms have been verified to reflect conditions likely to result in functional limitations, it is important to note that they only capture diagnosed disability, and not self-reported activity limitations or participation restrictions. Therefore, it will be important in the future to link administrative health data with other sources of information on disability such as disability-related income supports, or to add questions about disability (e.g., mobility, vision, hearing, cognition, self-care, or independent living) to COVID-19-related surveillance systems, including vaccination uptake data.
For example, it is possible to look at vaccination rates for people with intellectual and developmental disabilities (IDD), using some of these methods. Figure 4 is a bar graph summarizing COVID-19 vaccination uptake (at least first dose) for adults with IDD (n=96,465) broken down by age group, relative to adults without IDD (n=12,064,929) in the Ontario population as of June 7, 2021. Overall, 65% of adults with IDD have received their first vaccine compared to 69% of the general population. Vaccination rates are slightly higher for adults with IDD across age groups. However, differences are not as great as one might expect given that all adults with IDD, regardless of age, were prioritized as a high-risk group during Phase 2 and adults under age 40 without disabilities were only invited to register provincially in Phase 3. It is worth noting that the overall rate is lower for individuals with IDD despite rates being higher across age groups with IDD. This is because the age distribution of adults with IDD is younger, on average, than the general population, and so unvaccinated young people make up a greater proportion of the population with IDD than without IDD.
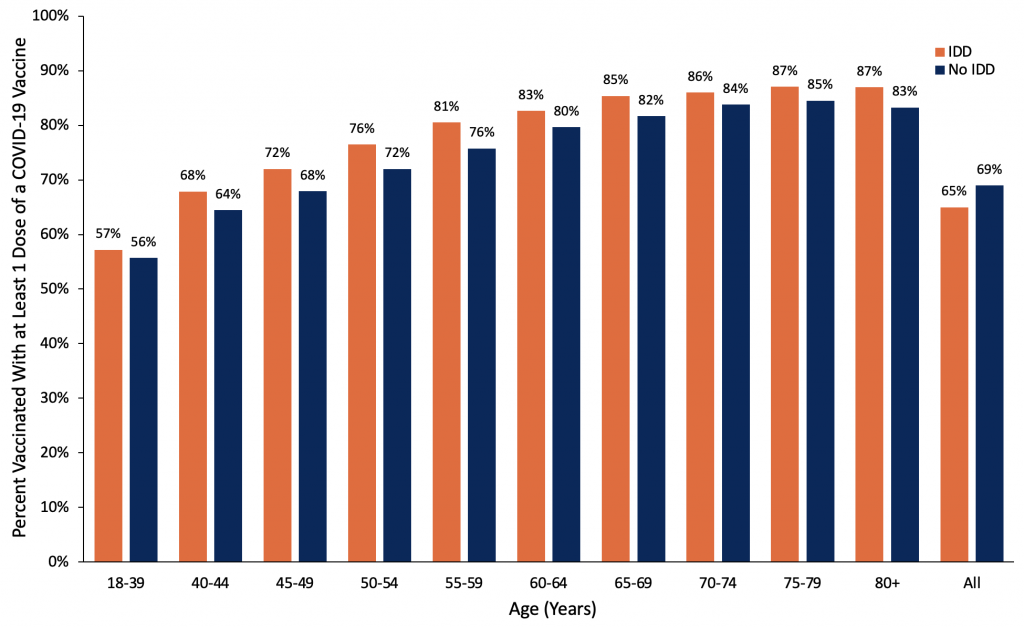
Bar graph presenting the percentage of Ontario adults with IDD, with at least one dose of COVID-19 vaccine, by age, as compared to Ontario adults without IDD, from December 15, 2020, to June 7, 2021. IDD, intellectual or developmental disabilities.
Figure 5 illustrates how vaccination rates by disability group can be monitored over time, to assess where gaps are, and indicate the impact of targeted initiatives. The figure shows a line graph measuring the proportion of all adults with IDD (n=96,465) vaccinated with at least one dose by age group each week between March 29 and June 7, 2021. Overall, cumulative coverage increased from 12% with one dose to 65%. Adults with IDD aged 65 years and older saw the greatest increase in vaccination rates earlier in the observation window, as compared to younger age groups.
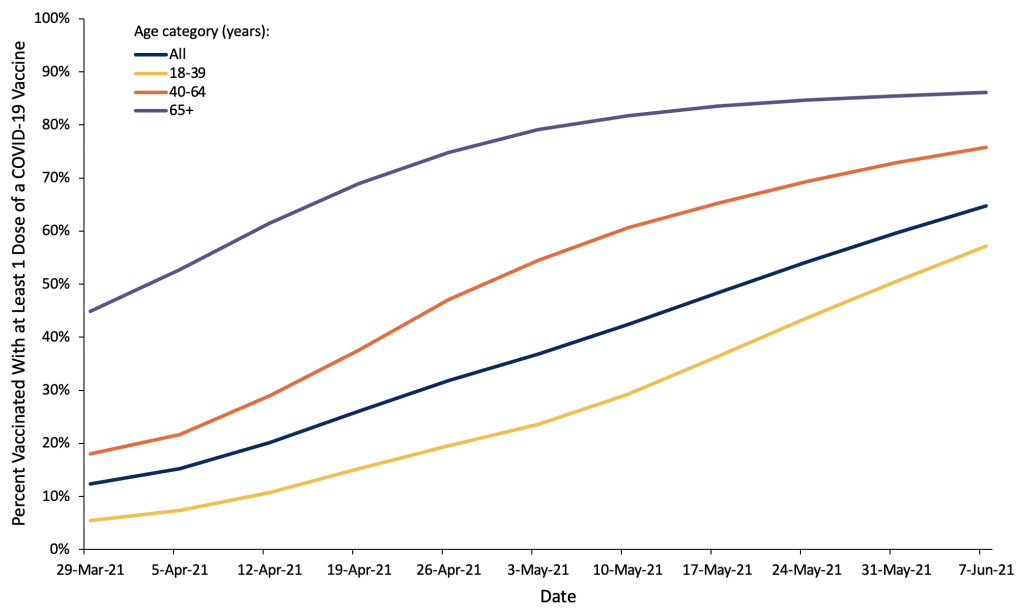
Line graph presenting the percentage of Ontario adults with IDD with at least one dose of COVID-19 vaccine, by age, from March 29 to June 7, 2021. IDD, intellectual or developmental disabilities.
Interpretation
People with disabilities are prioritized for COVID-19 vaccination in Ontario, yet there are still many barriers to universal access. As of May 7, 2021, PHU websites provided public information about 28% of critical accessibility features of vaccination locations, on average. Recognizing that websites are just one way of informing about accessibility and that websites are dynamic and continually updated as new information and appointments become available, this serves as an illustration of perceived accessibility at one point in time. It would be important complement this index of perceived accessibility with other measures, such as through obtaining feedback on accessibility from people with disabilities.
There are several steps that could be taken in the realms of communication, physical accessibility, and the social and sensory environment to reduce barriers to vaccination clinics, including training staff to support people with disabilities in getting vaccinated. Even if accommodations are available upon request, by phone, or at specific clinics, the lack of availability in multiple formats of this information may create barriers or discourage some individuals with disabilities from seeking vaccination. Many of these considerations are no- or low-cost (i.e., pen and paper for communication, no requirement/burden to offer proof of disability, rapid line for people with disabilities, etc.) or can be made with easy adaptations (i.e., selecting accessible locations when booking the vaccine, noting on the website that mobility devices are available to be used at clinics, or mentioning that there is an option to stay in-place for the 15 minutes following vaccination). Table 5 highlights measures that could be effective in improving the accessibility of Ontario’s COVID-19 vaccination both in the immediate future as well as in the medium-term.
| Immediate | Medium-Term | |
| Population-Level Benefits | Information about accessibility available on all PHU and vaccination clinic websites. Accommodation request form and other navigational supports with contact information available during booking process. Designated ‘Accessibility Champion’ available at each clinic. |
Publicly reported disability-disaggregated vaccination uptake data. Primary care vaccination programs for people with disabilities who require a more tailored and familiar response. Enhanced accessibility resources on PHU websites (vaccination clinic picture/video walk-through, accessible websites, standardized, accessible booking, etc.). Specialized disability training for vaccine clinic staff. |
| Targeted Approaches | Specialized clinics for people with disabilities. Drive-through clinics advertised to people with disabilities. Pop-up clinics include contact number to address accessibility requests and provide information on accessibility. |
Mobile in-home vaccination for hardest to reach people with disabilities. Outreach to support people with disabilities in booking and preparing for vaccination, in partnership with community organizations. |
Table highlighting measures that could be effective in improving the accessibility of Ontario’s COVID-19 vaccination both in the immediate future as well as in the medium-term.
Given the substantial risks of contracting SARS-CoV-2, higher rates of adverse outcomes from COVID-19, and social impacts of the pandemic on people with disabilities, vaccination is critical for Ontarians with disabilities. Therefore, using these findings to monitor and improve accessibility and shorten second dose intervals to better protect this at-risk population are critical steps moving forward. To implement these considerations, Ontario should use a two-pronged approach: improve general accessibility for mass-clinics and community pop-up clinics and use targeted approaches to reach people with disabilities through partnerships with community organizations, disability groups and health providers.40
Second Dose Considerations
While the focus has been to offer the first vaccination to as many people as possible, these data and lessons on accessibility are particularly salient for improving the second dose experience. Ontario previously extended the COVID-19 dose interval for up to 16 weeks to maximize the number of Ontarians receiving first doses, except for those with reduced immunological response and some very high risk individuals.18,41,42 With current vaccine supply, people with disabilities included in the highest-, high-, and at-risk and congregate setting Phase 2 groups should be prioritized for early second doses amongst those now eligible to rebook expedited second doses. For example, some people with disabilities living in congregate care outside of LTC have similar clinical characteristics and setting-based risk factors that enhance their risk of contracting SARS-CoV-2. These settings have experienced similar restrictions and COVID-19 outbreaks but have not yet been given an expedited dose schedule shorter than the 16-week interval. Given the substantial restrictions placed on these settings (i.e., minimal in-person contact with family, cessation of regular activities, etc.), the mental health impacts, and continued outbreaks, there are marked benefits to reducing the interval to the second dose. Several other jurisdictions have recently shifted their policy to include some people with disabilities for prioritized second doses, such as people with Down syndrome and those living in disability based congregate care in Manitoba, all adults deemed ‘clinically extremely vulnerable’ in BC, and people in the equivalent of Ontario’s highest-, high-, and at-risk categories in the UK.43,44
Furthermore, certain disabilities are associated with reduced immune system function, while some neuromuscular conditions that impact respiratory function are already associated with high mortality rates from breathing disorders, including pneumonia and influenza,45 despite annual access to the influenza vaccine. These individuals have been in the highest risk provincial categories and many have not left their homes or socialized since the pandemic began, leading to substantial negative impacts on their mental health and that of their caregivers. An estimated 83% of disabled Canadians said that the pandemic has negatively impacted their mental health, while 80% report greater social isolation.16,46 Given the significant risk, social harms of prolonged isolation, and lack of evidence of sufficient protection after one dose for these populations, when vaccine supply allows, people with disabilities already included in the highest-, high, and at-risk groups listed in Phase 2 should be prioritized for earlier second doses of COVID-19 vaccine and supported to rebook appointments.
Monitoring Vaccine Distribution Among People with Disabilities
Publicly available data on COVID-19 vaccination rates for people with disabilities at the provincial and PHU levels are important metrics, given that many people with disabilities fall into the provincially designated highest, high, and at-risk categories. The example provided of COVID-19 vaccination rates for people with intellectual or developmental disabilities through linked health administrative data held at ICES, could be expanded to include other disability groups to better understand how Ontario is reaching people with disabilities. Given the high-risk nature of this group, one might have expected a sustained increase over time in all groups, in Figure 5, rather than increases in vaccination rates associated with provincial age group eligibility. While there are limitations when studying a population using health administrative data, it can offer some insights into inequities and can be combined with other data collection efforts, such as including the tracking of disability within the COVaxON system itself, or the monitoring of vaccination rates for Ontario Disability Support Plan or Ontario Assistive Device Program recipients. As vaccinations are extended to children and youth with disabilities, tracking information could be collected in conjunction with other child-based data collection efforts. Public monitoring of vaccination information could be part of a broader disability-based data reporting strategy which could also include the sharing of data on disability specific testing, positivity rates, and COVID-19 related hospital use and mortality. In addition to monitoring vaccination rates, there should be mechanisms including an accessible feedback form and a helpline to assist, monitor and improve the overall accessibility of vaccination for Ontarians with disabilities.
Methods Used for This Science Brief
The description of PHU accessibility was based on a scan of all Ontario PHU websites performed on May 7, 2021. At each PHU website, information was extracted based on three accessibility categories in the framework: physical accessibility, communication for accessibility, and social/sensory environment. Specifically, for each category, the following information was extracted:
- Communication: accessible website; multiple booking options; phone number available; sign language interpretation; information about requirements to move between stations in the vaccination centre; second appointment provided during first appointment.
- Physical Accessibility: ability to book appointments for pop-up clinics; private booths available; accessible entrance at site; wheelchair available on site; accessible post-vaccination waiting area; drive-through available; mobile in-home vaccination offered.
- Social/Sensory Environment: ability to bring a care partner; specialized clinic or hours for people with disabilities; no requirement/burden to offer proof of disability; ability to move around while waiting during the observation period; face mask exemption policy in place.
Website accessibility was checked using the WAVE web accessibility evaluation tool, which measures the number of items that do not meet Web Content Accessibility Guideline (WCAG) accessibility standards. The tool provides a number of total errors, and the total score and the number of contrast errors were used in this analysis.
To analyze information about COVID-19 vaccine distribution for adults with intellectual or developmental disabilities, health administrative records from various databases were linked using unique encoded identifiers and analyzed at ICES. ICES is a non-profit, independent organization that reports on the health and health care utilization of Ontario residents. Data stored at ICES were in an anonymized format before they were accessed by the authors. All datasets were linked using unique encoded identifiers and analyzed at ICES. The use of data in this project was authorized under section 45 of Ontario’s Personal Health Information Protection Act, which does not require review by a Research Ethics Board.
Adults aged 18 years and older were considered to have intellectual or developmental disabilities if a diagnosis of intellectual disability, fetal alcohol syndrome, autism, and/or other pervasive developmental disorders and chromosomal and autosomal anomalies (i.e., Down syndrome, Fragile X syndrome) was recorded in health administrative databases held at ICES. To be included in this IDD group, they had to have these diagnoses recorded in either ≥ 2 physician visits (Ontario Health Insurance Plan, OHIP) or ≥ 1 ED visit (National Ambulatory Care Reporting System, NACRS) or hospitalization (Discharge Abstract Database, DAD or Ontario Mental health Reporting System, OMHRS) since birth or inception of each database (whichever occurred later) until June 7, 2021. More details on diagnostic codes capturing intellectual or developmental disabilities can be found here.47 Reliance on administrative health data only to create a cohort of adults with intellectual or developmental disabilities may not include all such adults.
Vaccination results were recorded in COVaxON between December 15, 2020, and June 7, 2021.
- Statistics Canada. A demographic, employment and income profile of Canadians with disabilities aged 15 years and over, 2017. Government of Canada. Published November 28, 2018. Accessed May 18, 2021. https://www150.statcan.gc.ca/n1/pub/89-654-x/89-654-x2018002-eng.htm
- Human Resources and Skilld Development Canada. Federal disability reference guide. Government of Canada. Published April 11, 2013. https://www.canada.ca/en/employment-social-development/programs/disability/arc/reference-guide.html
- Office for National Statistics. Coronavirus (COVID-19) related deaths by disability status, England and Wales: 2 March to 14 July 2020. ons.gov.uk. Published 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbydisabilitystatusenglandandwales/2marchto14july2020
- Office for National Statistics. Updated estimates of coronavirus (COVID-19) related deaths by disability status, England: 24 January to 20 November 2020. ons.gov.uk. Published 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbydisabilitystatusenglandandwales/24januaryto20november2020
- Gleason J, Ross W, Fossi A, Blonsky H, Tobias J, Stephens M. The devastating impact of Covid-19 on individuals with intellectual disabilities in the United States. NEJM Catal. Published online March 5, 2021:12. https://doi.org/10.1056/CAT.21.0051
- The OpenSAFELY Collaborative, Williamson EJ, McDonald HI, et al. OpenSAFELY: Risks of COVID-19 Hospital Admission and Death for People with Learning Disabilities – a Cohort Study. Infectious Diseases (except HIV/AIDS); 2021. https://doi.org/10.1101/2021.03.08.21253112
- Clift AK, Coupland CAC, Keogh RH, Hemingway H, Hippisley-Cox J. COVID-19 mortality risk in Down syndrome: Results from a cohort study of 8 million adults. Ann Intern Med. 2020;174(4):572-576. https://doi.org/10.7326/M20-4986
- Nemani K, Li C, Olfson M, et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiatry. 2021;78(4):380. https://doi.org/10.1001/jamapsychiatry.2020.4442
- Salter A, Fox RJ, Newsome SD, et al. Outcomes and risk factors associated with SARS-CoV-2 infection in a North American registry of patients with multiple sclerosis. JAMA Neurol. Published online March 19, 2021. https://doi.org/10.1001/jamaneurol.2021.0688
- García-Azorín D, Martínez-Pías E, Trigo J, et al. Neurological comorbidity is a predictor of death in Covid-19 disease: A cohort study on 576 patients. Front Neurol. 2020;11. https://doi.org/10.3389/fneur.2020.00781
- Public Health England. Deaths of People Identified as Having Learning Disabilities with COVID-19 in England in the Spring of 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/933612/COVID-19__learning_disabilities_mortality_report.pdf
- Wong A, Landes S. COVID-19 risk for individuals with intellectual and/or developmental disabilities varies by type of residential setting. Lerner Cent Public Health Promot Popul Health Res Brief Ser. Published online January 5, 2021. https://surface.syr.edu/lerner/111
- Landes SD, Turk MA, Wong AWWA. COVID-19 outcomes among people with intellectual and developmental disability in California: The importance of type of residence and skilled nursing care needs. Disabil Health J. 2021;14(2):101051. https://doi.org/10.1016/j.dhjo.2020.101051
- Centers for Learning, Research & Innovationin Long-Term Care. A Home for All: Younger Residents Living in Long-Term Care. Ontario CLRI Accessed May 18, 2021. https://clri-ltc.ca/files/2019/01/Younger-Residents-in-LTC-Handout.pdf
- IC/ES. COVID-19 Dashboard. Published April 6, 2021. Accessed April 7, 2021. https://www.ices.on.ca/DAS/AHRQ/COVID-19-Dashboard
- Martin K, Gee C, Hoekstra F, et al. COVID-19 Disability Survey. Abilities Centre; 2020:21. https://abilitiescentre.org/Abilities/media/Documents/Covid-survey-report-Dec-18_1.pdf
- Shakespeare T, Ndagire F, Seketi QE. Triple jeopardy: disabled people and the COVID-19 pandemic. The Lancet. 2021;397(10282):1331-1333. https://doi.org/10.1016/S0140-6736(21)00625-5
- McGrath JM. Here’s Ontario’s May 12 vaccine update. TVO.org. Published May 12, 2021. https://www.tvo.org/article/heres-ontarios-may-12-vaccine-update
- McKee M, Okanlami O, Zazove P. Guidelines for Accessible COVID-19 Testing & Vaccination Sites. Ann Fam Med COVID-19 Collect. Published online February 17, 2021. https://doi.org/10.7302/231
- Courtenay K, Perera B. COVID-19 and people with intellectual disability: impacts of a pandemic. Ir J Psychol Med. 2020;37(3):231-236. https://doi.org/10.1017/ipm.2020.45
- Spaul SW, Hudson R, Harvey C, Macdonald H, Perez J. Exclusion criterion: learning disability. The Lancet. 2020;395(10223). https://doi.org/10.1016/S0140-6736(20)30051-9
- Illouz T, Biragyn A, Frenkel-Morgenstern M, et al. Specific susceptibility to COVID-19 in adults with Down Syndrome. NeuroMolecular Med. Published online March 4, 2021. https://doi.org/10.1007/s12017-021-08651-5
- W3C Web Accessibility Initiative (WAI). Web Content Accessibility Guidelines (WCAG) Overview. Web Accessibility Initiative (WAI). Published 2021. https://www.w3.org/WAI/standards-guidelines/wcag/
- Weikle B. Made-in-Canada solution: “Hockey hub” vaccine clinics are getting the job done faster. CBC Radio. Published May 22, 2021. Accessed May 23, 2021. https://www.cbc.ca/radio/whitecoat/made-in-canada-solution-hockey-hub-vaccine-clinics-are-getting-the-job-done-faster-1.5953312
- Choi KH, Denice P, Haan M, Zajacova A. Studying the social determinants of COVID-19 in a data vacuum. Can Rev Sociol Can Sociol. Published online 2021. https://doi.org/10.1111/cars.12336
- Huynh T. Hot spot tracker. The Local. Published May 14, 2021. Accessed May 12, 2021. https://thelocal.to/hot-spot-tracker/
- Carter A. COVID-19 vaccine rollout improving in hardest-hit areas but inequities remain, research shows | CBC News. CBC. Published April 23, 2021. https://www.cbc.ca/news/canada/toronto/covid-toronto-vaccination-rates-neighbourhoods-1.6000197
- Kelly D. Southlake, Mackenzie Health, Reena partner to vaccinate residents with developmental disabilities. NewmarketToday.ca. Published March 5, 2021. https://www.newmarkettoday.ca/local-news/southlake-mackenzie-health-reena-partner-to-vaccinate-residents-with-developmental-disabilities-3744773
- Yousif N. CAMH urges province to send more COVID-19 vaccine after dwindling supply forces closure of clinic for mentally ill, disabled. thestar.com. Published April 30, 2021. https://www.thestar.com/news/gta/2021/04/30/camh-urges-province-to-send-more-covid-19-vaccine-after-dwindling-supply-forces-closure-of-clinic-for-mentally-ill-disabled.html
- Wong C. COVID-19 vaccine clinic pops up for weekend in Kitchener. Kitchener. Published March 27, 2021. https://kitchener.ctvnews.ca/covid-19-vaccine-clinic-pops-up-for-weekend-in-kitchener-1.5365207
- City of Toronto. City of Toronto and partners increase vaccine access and uptake for vulnerable residents through community mobilization and engagement. City of Toronto. Published May 12, 2021. https://www.toronto.ca/news/city-of-toronto-and-partners-increase-vaccine-access-and-uptake-for-vulnerable-residents-through-community-mobilization-and-engagement/
- Henry M. Families of medically fragile children ‘so excited’ to end a year of high anxiety with long-awaited jab. thestar.com. Published May 22, 2021. Accessed May 23, 2021. https://www.thestar.com/news/gta/2021/05/22/families-of-medically-fragile-children-so-excited-to-end-a-year-of-high-anxiety-with-long-awaited-jab.html
- Kiran T. Why have family doctors been overlooked in vaccine rollout? thestar.com. Published March 5, 2021. https://www.thestar.com/opinion/contributors/2021/03/05/why-have-family-doctors-been-overlooked-in-vaccine-rollout.html
- Stall NM, Nakamachi Y, Chang M, et al. Mobile in-home COVID-19 vaccination of Ontario homebound older adults by neighbourhood risk. Sci Briefs Ont COVID-19 Sci Advis Table. 2021;1(19). https://doi.org/10.47326/ocsat.2021.02.19.1.0
- Huynh T, Sava N, Hahn-Goldberg S, et al. Mobile on-site COVID-19 vaccination of naturally occurring retirement communities by neighbourhood risk in Toronto. Sci Briefs Ont COVID-19 Sci Advis Table. 2021;1(14). https://doi.org/10.47326/ocsat.2021.02.14.1.0
- Eliminating barriers through mobile COVID-19 vaccine clinic. Published April 7, 2021. https://www.cbc.ca/player/play/1882291267587
- Brown HK, Ray JG, Chen S, et al. Association of Preexisting Disability With Severe Maternal Morbidity or Mortality in Ontario, Canada. JAMA Netw Open. 2021;4(2):e2034993. https://doi.org/10.1001/jamanetworkopen.2020.34993
- Brown HK, Carty A, Havercamp SM, Parish S, Lunsky Y. Identifying reproductive-aged women with physical and sensory disabilities in administrative health data: A systematic review. Disabil Health J. 2020;13(3):100909. https://doi.org/10.1016/j.dhjo.2020.100909
- Lin E, Balogh R, Cobigo V, Ouellette-Kuntz H, Wilton AS, Lunsky Y. Using administrative health data to identify individuals with intellectual and developmental disabilities: a comparison of algorithms. J Intellect Disabil Res. 2012;57(5):462-477. https://doi.org/10.1111/jir.12002
- Health Care Access Research and Developmental Disabilities. Including people with developmental disabilities as a priority group in Canada’s COVID-19 vaccination program: key considerations: Part 2. Published March 29, 2021. https://www.porticonetwork.ca/web/hcardd/news/-/blogs/including-people-with-developmental-disabilities-as-a-priority-group-in-canada-s-covid-19-vaccination-program-key-considerations-part-2
- Ministry of Health. Extension of the Second Dose Interval. Government of Canada; 2021. https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/vaccine/COVID_19_vaccine_dose_intervals.pdf
- Ministry of Health. Vaccine Clinical Advisory Group (VCAG) Recommendations on Exceptions to Extended Dose Intervals for COVID-19 Vaccines. Government of Canada; 2021:9. https://www.health.gov.on.ca/en/pro/programs/publichealth/coronavirus/docs/vaccine/COVID_19_medical_exceptions_vaccine_dose_intervals.pdf
- Government of Manitoba. Province of Manitoba: Second dose eligibility. Province of Manitoba. https://www.gov.mb.ca/covid19/vaccine/eligibility-criteria.html
- BC Centre for Disease Control. Vaccine considerations. bccdc.ca. Published May 13, 2021. http://www.bccdc.ca/health-info/diseases-conditions/covid-19/covid-19-vaccine/vaccine-considerations
- Benditt JO, Boitano LJ. Pulmonary issues in patients with chronic neuromuscular disease. Am J Respir Crit Care Med. 2013;187(10):1046-1055. https://doi.org/10.1164/rccm.201210-1804CI
- Pettinicchio D, Maroto M, Chai L, Lukk M. Findings from an online survey on the mental health effects of COVID-19 on Canadians with disabilities and chronic health conditions. Disabil Health J. Published online February 24, 2021:101085. https://doi.org/10.1016/j.dhjo.2021.101085
- Lunsky Y, Klein-Geltink JE, Yates EA. H-CARDD Cohort Cerivation: An Overview. ICES & CAMH; 2013. https://www.ices.on.ca/flip-publication/Atlas-on-the-Primary-Care-of-Adults-with-Developmental-Disabilities/files/assets/basic-html/index.html#165
Author Contributions: SR conceived the Science Brief. SR and YL wrote the first draft of the Science Brief. SR, JC, SC, YS, and GMK collected the data on PHUs, and MD performed analyses of PHU website reviews. Vaccination rate analysis was performed at ICES and interpreted by HKB and YL. All authors revised the Science Brief critically for important intellectual content and approved the final version.
The ICES analysis was supported by the Applied Health Research Questions (AHRQ) Program at ICES, which is funded by the Ontario Ministry of Health, and by the Ontario Health Data Platform (OHDP), a Province of Ontario initiative to support Ontario’s ongoing response to COVID-19 and its related impacts. Parts of this material are based on data and information compiled and provided by Ontario Ministry of Health, the Canadian Institute for Health Information and Public Health Ontario. The analyses, conclusions, opinions, and statements expressed herein are those of the authors and do not reflect those of ICES, OHDP, or the funding or data sources; no endorsement is intended or should be inferred. We would like to acknowledge Public Health Ontario for access to case level data from iPHIS Plus and COVID-19 laboratory data, as well as assistance with data interpretation. We also thank the staff of Ontario’s PHUs who are responsible for COVID-19 case and contact management and data collection within iPHIS Plus.
Citation: Rotenberg S, Downer MB, Brown HK et al. COVID-19 Vaccination for People with Disabilities. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(35). https://doi.org/10.47326/ocsat.2021.02.35.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
Please contact info@covid19-sciencetable.ca if you have any questions or require communications support.
