Effective Modalities of Virtual Care to Deliver Mental Health and Addictions Services in Canada
Authors:Brian Lo, Gillian Strudwick, Linda Mah, Christopher J. Mushquash, Kwame McKenzie, Akwatu Khenti, Allison Crawford, Onil Bhattacharya, Upton Allen, Nicolas S. Bodmer, Karen B. Born, Anna Perkhun, Fahad A. Razak, Braden O’Neill on behalf of the Mental Health Working Group and the Ontario COVID-19 Science Advisory Table
Key Message
The delivery of virtual mental health care by regulated healthcare professionals has grown substantially since the onset of the COVID-19 pandemic. In the limited research conducted on this modality, virtual mental health care has been found to be efficacious for supporting patients with depression, anxiety, and post-traumatic stress disorder. However, there is limited comparative evidence between in-person and virtual modalities, or for severe mental illnesses such as schizophrenia or bipolar disorder. Thus, despite the surge in the use of virtual care during the pandemic, it is important to recognize that virtual care may not be an adequate substitute for in-person treatment for all populations or conditions. Further, while virtual mental health care has the potential to address barriers to access to care for rural and underserved communities, it may also propagate existing inequities in mental health care for under-resourced populations. Many challenges to the delivery of equitable care through virtual mental health remain. Enhancing technological literacy and access for clinicians and clients, and delivering culturally competent care that aligns with the needs of the local population and community is a largely unaddressed priority for advancing transparency, trust and equity.
Deliberate consideration of the specific needs and issues, preferences, culture and values of individual patients and communities is important to deliver culturally-competent virtual mental health models of care for equitable, accessible recovery. This should be done through close engagement and collaborative co-creation with patients, mental health researchers, practitioners and communities.
Summary
Background
Virtual mental health care, delivered by a regulated health professional in a synchronous manner, has experienced unprecedented growth in the last two years during the COVID-19 pandemic. Its benefits and widespread use by Ontarians have suggested a need to examine the current evidence and identify policy recommendations to enhance the delivery of quality virtual mental health care.
The current brief focuses on the synchronous delivery of virtual mental health care to adults by regulated health care professionals. While there is a growing number of self-help and asynchronous tools (e.g., internet-delivered cognitive behavioural therapy), evidence about these tools is outside the scope of this brief.
Questions
To what extent is virtual mental health care efficacious for improving outcomes?
What are the unique considerations and needs to make virtual mental health care effective for particular groups and communities (e.g., Indigenous populations)?
What is required for quality selection and delivery of virtual mental health care by health care professionals in the clinical environment?
Findings
Overall, virtual mental health care has been found to be efficacious for depression, anxiety and post-traumatic stress disorder in comparison to in-person care. However, there is limited evidence on its use for assessment, education and cognitive rehabilitation for individuals suffering from severe mental illness.
While there has been growing discussion on delivering virtual mental health care and its intersectionality with various racialized and/or marginalized groups, including Black, rural and First Nations, Inuit and Métis communities, some of the communities are still challenged by a lack of housing, privacy, digital literacy support and high-speed internet and technology infrastructure and/or costs. Moreover, current services may not provide culturally relevant care that is critical for the diverse populations of Ontario. In particular, there is a need to examine how the social determinants of health can influence access to virtual mental health care and data literacy.1,2 Other jurisdictions have demonstrated that involving communities at all stages of developing virtual care services, ensuring Indigenous leadership, and partnering to develop and deliver culturally-relevant care are all necessary to create quality virtual mental health services.3–5
Current guidance on appropriate selection and use of virtual care has primarily been developed for provision of virtual care outside of a mental health context, and has suggested careful consideration of the clinical presentation, the patient’s preference and their needs and ability to access virtual mental health care.
Interpretation
Virtual delivery of mental health care should continue to have a strong presence after the pandemic period in the Ontario health system, given its efficacy, acceptability and feasibility. However, until comparative effectiveness evidence is available, in-person options should continue to remain available for various clinical situations. Careful coordination of local and regional planning of resources is needed to ensure delivery of care that fits the local context. Engaging and partnering with individuals, families and community organizations is necessary to ensure that sustainable and quality care is delivered across the province. In addition, there is a need to consider the diverse needs, preferences and values of communities for culturally competent virtual mental health care. This may be facilitated through deliberate engagement, training, guidance and support on virtual mental health care for patients, families and healthcare professionals. Moreover, developing a unified quality standard is important to guide appropriate selection and delivery of virtual mental health care to the province. Lastly, investing in the expansion of appropriate infrastructure (e.g., digital literacy support, access to high-speed internet) is required.
Background
The COVID-19 pandemic has led to widespread interest in and adoption of virtual care (or telemedicine).6–8Virtual Mental Health Care is defined as the delivery of mental health care through and with the use of information communication and technology (ICT) tools at a distance.9 This can include the delivery of psychotherapy, consultation, and medication management. There has been considerable discussion about the delivery of virtual care in a synchronous or asynchronous approach using telephone, text messaging, teleconferencing platforms (e.g., Zoom, MS Teams), and mobile apps.10,11 However, given the current interest in synchronous (live) delivery of care (e.g., assessment, treatment, consultations) led by mental health care professionals, this briefing note will align with the definition from Ontario Health9 and Canadian Medical Association,12 and focus on synchronous delivery of virtual mental health care and cite only literature related to this modality.
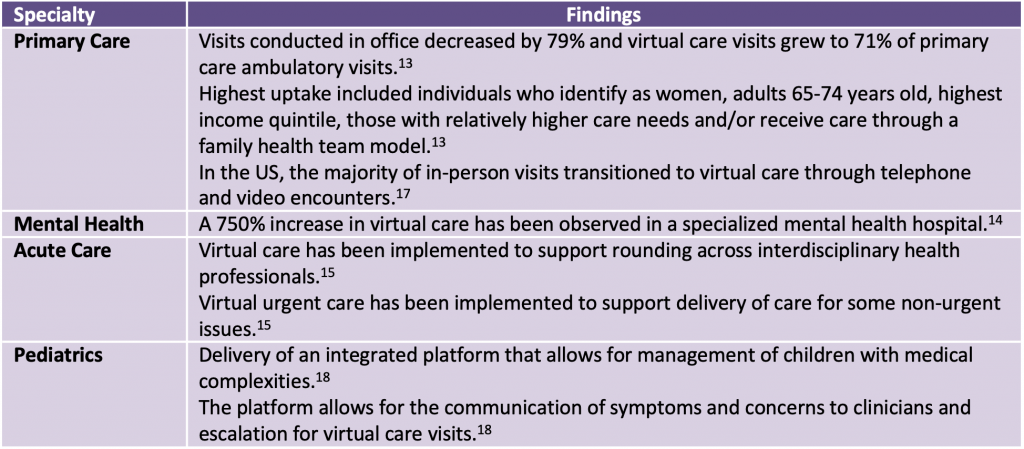
In primary care, a 56-fold increase in virtual care visits has been observed in Ontario,13 and similar trends have been observed for specialized mental health settings.14 With the ability for patients and families to access care from home, virtual care has been widely discussed in urgent and emergency care,15,16 primary care,13,17 and pediatrics (Table 1).18 However, there is limited consolidation of best practices and recommendations for use of virtual modalities19 in the delivery of mental health care in Canada. Mental health care is unique given the importance of developing a therapeutic rapport and longitudinal relationships with clients.20 In particular, mental health care is most effective when delivered through multi-faceted, team-based approaches that may include psychotherapists, social workers, case workers, primary care physicians, pharmacists and nurses.21,22 In some cases, as physician involvement can be more limited than other specialties (e.g., only to assessments and consultations), the model of care and approach towards the use of virtual modalities can be quite different.23 Given the interest in the ongoing use of virtual care beyond the pandemic and growing concerns related to compassionate care24 and equitable delivery of virtual care,25there is a timely and critical need to review current evidence and identify policy recommendations to enhance sustainable, effective delivery of virtual mental health care in Ontario beyond the COVID-19 pandemic. In particular, there is a need to look at lived experience and engage with underserved communities, including Black, Indigenous and other racialized communities, to better understand how these populations view mental illness and the recovery process in order to co-create services that meet their needs.
Impact of Pandemic on Virtual Care Use in Mental Health
There has been substantial uptake and adoption of virtual modalities for mental health care delivery. Bhatia et al. reviewed administrative data in Ontario and found that virtual ambulatory visits grew significantly when the pandemic began and reached as high as 70% of all outpatient visits in the second quarter of 2020.7 Notably, mental health issues were cited to account for the highest proportion of virtual visits.7 The majority of virtual visits used the telephone, and only 8.8% of all visits were video visits.7 Similarly, administrative data from OHIP billing data suggests that psychiatry continues to be one of the highest adopters of virtual care visits .26Canada Health Infoway examined virtual care offerings to patients through a survey of ~1,500 Canadians across the country and found that about half reported being offered virtual care options for their visit.27 About a third of those individuals chose to do their visit virtually, with a substantial proportion (47%) of these individuals reporting that they wanted to do it using videoconferencing. The Canadian Institute for Health Information (CIHI) estimated that about 244 services per 1000 Canadians per month were conducted through virtual modalities since the onset of the pandemic and the rapid adoption of virtual care was observed regardless of income level and province.28 As Canadians adopt more digital technologies, it is expected that virtual care will continue to have a significant role in mental health care moving forward. Thus, in order to realize the benefits of virtual care, it is important to address some of the current concerns of virtual mental health care related to privacy, commodification of marginalized communities and access.29
Questions
To what extent is virtual mental health care efficacious for improving outcomes?
What are the unique considerations and needs to make virtual mental health care effective for particular groups and communities (e.g., Indigenous populations)?
What is required for quality selection and delivery of virtual mental health care by health care professionals in clinical environments?
Findings
Efficacy of Virtual Mental Health Care
There has been considerable work in the last two years looking at the efficacy and patient satisfaction with virtual mental health care in adults prior to the pandemic, including a rapid review on this topic from the McMaster Health Forum.30 While public and clinician preferences and perceptions towards virtual care have shifted since the onset of the pandemic, this literature provides the foundation for understanding its efficacy to date. In that rapid review, of the 31 literature reviews that were identified, 26 focused on the delivery of virtual mental health care to adults and the reviews ranged from narrative reviews to meta-analyses.30 Overall, the authors concluded that virtual psychotherapy was as efficacious as in-person care for individuals with a diagnosis of depression, anxiety, or post-traumatic stress disorder.30 One systematic review and meta-analysis found 14 randomized controlled trials (RCTs) comparing videoconferencing and in-person counselling and reported that videoconferencing was not inferior to in-person care.31 However, 12 RCTs comparing these two modalities for psychiatric assessments had inconclusive findings.31 Notably, many of these systematic reviews had very few studies originating from Canada. More recently, studies looking at video neuropsychological assessments found that despite an overall good agreement with the in-person rating of the assessments, there is limited validation and standards for conducting these assessments virtually.32–34
For patients diagnosed with severe mental illness (e.g., eating disorders, psychosis), a systematic review led by Lawes-Wickwar et al. in 2018 found that of the 31 articles identified (29 comparative trials), there is inconclusive evidence on the efficacy of virtual mental health care for cognitive rehabilitation, patient education and assessment.30,35 This is similar to a rapid review conducted on use of virtual modalities of care for treatment of schizophrenia.36 However, two systematic reviews examining the acceptability of digital tools, including virtual mental health care, found that there is high acceptability of these modalities among those with severe mental illness.37,38 Similarly, the evidence brief from the McMaster Health Forum30 also highlighted the ability of virtual mental health care in promoting medication adherence. There was no evidence of the use of virtual mental health care for substance use assessment and management.30
There is also evidence that the virtual delivery of mental health care is efficacious for reducing psychological symptoms secondary to chronic diseases39 and neurocognitive disorders.33 In a knowledge synthesis conducted for CIHR, Gagnon et al. found that digital health tools, including virtual mental health care, can be useful for supporting the mental health needs of those managing chronic diseases (e.g., cancer).39 Similarly, another systematic review on neurocognitive disorders found that virtual mental health care can address some of the challenges exacerbated by the pandemic.33
There have also been some studies looking at patient experience of virtual mental health care. A systematic review looking at the use of virtual mental health care by patients suffering from dementia found that the patient experiences were overall positive and they remain interested in using the service.33 This is significant considering the profound impact that the pandemic has had on this population including exacerbation of symptoms (e.g., fear, memory, anxiety, psychotic symptoms) and interruption of the multi-faceted therapeutic plan required for this condition.33 However, in terms of telephone-delivered virtual mental health care, a systematic review by Coughtrey and colleagues,40 which included 14 studies (RCTs and quasi-experiments), found that while telephone-delivered care reduced symptoms of depression and anxiety among patients, the use of virtual delivery of mental health care could lead to more limited therapeutic relationship when compared to in-person care. There is growing recognition of some differences in outcomes that matter to patients related to virtual mental health care.41 In the ‘Canadian Digital Health Survey’ led by Canada Health Infoway, over 90% of respondents who indicated they had a virtual care visit felt satisfied. However, only 40% of these individuals would actively promote virtual care to others. Similarly, several studies42 also highlighted some of the barriers that some experience in receiving virtual mental health care. This included completing assessments that would have been done in-person, ability to ask questions to the providers and developing the relationship with the clinician.
There is inadequate evidence comparing experiences and outcomes between different modalities of virtual care. Most importantly, given the frequent use of both modalities, there is very limited evidence comparing efficacy between telephone and video visits. In a Cochrane systematic review looking at telephone and video modalities in smoking cessation services, while individuals were more likely to recommend video consulting than telephone consulting, there were overall no differences in the therapeutic bond, satisfaction, and adherence to the treatment program.43 Understanding how these findings compare across racial and cultural demographics would also be needed. There is currently very limited data on the use of virtual care by persons with disabilities.
Use of Virtual Mental Health Care for Diverse Populations
There is increasing recognition that health technologies cannot be implemented without consideration of the cultural, social, and economic contexts in which they are used. While virtual care holds great promise for increasing access to mental health services, it can also deepen or create new health inequities; considerations such as availability of infrastructure, internet connectivity, housing, privacy, digital literacy, and cultural beliefs and values can all influence access, engagement, and satisfaction with care.25 There have been some preliminary discussions on supports that would be useful to support for those with mobility and hearing aids and others, such as providing audio-only options, having a family member be there to assist, or providing tips to prepare for a virtual visit.29,44 However, many populations continue to have challenges in receiving the mental health care they require such as people in urban settings with low-income levels,45 LGBTQ2S+ populations,46 indigenous populations47 and ethnocultural minorities.48 In particular, many Black and racialized populations have disparate social determinants of health (e.g., systemic racism, food and housing insecurity), which can further hinder their ability to utilize virtual mental health care services. The psychological safety and cultural safety of virtual care must also be considered, along with impacts on communities. Thus, an intersectional approach that is inclusive of the needs of vulnerable populations and communities is needed.1,49 Particular attention has already been focused on virtual care for rural communities, First Nations, Inuit and Métis communities, refugees, and older adults.
Black and Other Racialized Communities
While considerable work has been done on looking at the use of virtual mental health care, more work is required to understand how the delivery of these services can support the needs of Black and racialized communities in Canada. Thomeer and colleagues highlighted that during the COVID-19 Pandemic in the US, despite higher burden of mental health issues among Black, Hispanic and Asian populations, their needs were more likely to remain unmet in comparison to White respondents.50 Moreover, a report conducted by the Mental Health Commission of Canada and the Wellesley Institute looking at the mental health of racialized communities in Ontario during the pandemic highlighted the need for focused considerations of the social determinants of health and existing disparities to deliver culturally responsive virtual mental health services.51,52
Rural and Remote Communities
Virtual care represents a promising opportunity to improve access to health services in rural and remote areas which have a higher burden of mental health needs, coupled with health human resource shortages.53,54Many studies now establish the ability to receive quality mental health care in rural and remote settings through virtual care and to create evidence-based models of care that would otherwise be limited in rural these communities, such as collaborative care models in which specialists join the team virtually.55 Canadian studies have also found additional benefits, such as addressing mobility and transportation issues,56 and have shown that virtual care is less expensive than alternatives such as physician travel into communities, or patient travel to distal treatment centers.57 Virtual care in rural and remote Ontario has been shown, prior to the COVID-19 pandemic, to be particularly utilized by family health teams from rural areas, who tended to have patients with greater clinical complexity and mental health issues.58 After the onset of the COVID-19 pandemic, there were greater increases in the rate of virtual visits per 1000 people among primary care physicians in ‘capitation’ models as opposed to those providing care ‘fee-for-service’, and there were greater increases in urban than in rural practices.13 Rural and remote communities can have unique circumstances that can pose barriers to equitable access to virtual care, such as poor internet connectivity and relative lack of devices required for connectivity. There is also important work that must be done at a health systems level to ensure that there is a planful system of virtual care provision, or the risks are discontinuity of care, maldistribution of care, and service providers who are unfamiliar with the community, and cultures, and contexts in which they are providing care.58
First Nations, Inuit, and Métis Populations
Although it is widely recognized that the use of virtual care and other health technologies deserves careful consideration, there is currently limited and/or emerging evidence.59–62 Additionally, while almost half of Indigenous people live in rural or remote communities, more than half reside in urban settings.63 These contextual differences highlight the importance of unique considerations when developing approaches and policies for virtual care. A study by Laperrière et al. explored the impact of the COVID-19 pandemic, including the transition to virtual care, on Indigenous community members living in Ottawa-Gatineau, and found that the lack of internet and technology greatly complicated their ability to access virtual mental health care.64 Some key areas highlighted across the literature that require further attention: understanding that each community is unique and that there is great diversity among Indigenous Peoples and communities; ensuring that services are culturally safe and developed with leadership from First Nations, Inuit, and Métis communities and providers; and, considering the unique strengths of communities, as well as the ways that communities and individuals have been impacted by historical trauma and loss, and ongoing racism, including within healthcare. Thus, virtual care services should be equipped with providers that can provide culturally and contextually appropriate care to these populations.
Refugees
Refugees in Canada also reported suffering substantial barriers in access to virtual mental health care due to challenges with finding private spaces, developing trust with the provider and limitations of the technology (e.g., internet speed).65
Older Adults
A 2019 systematic review identified nine articles on the use of virtual mental health care for depression in older adults (65+ years old).56 Overall, it reported that while the use of virtual mental health care had an impact on health outcomes (e.g., depressive symptoms), numerous considerations should be made including their preferences for use of technology, their ability to communicate via the technology, and visual/auditory impairments.
Integrated Models of Virtual and In-Person Mental Health Care
While guidance for helping clinicians select the most appropriate modality for virtual mental health care is emerging, there is mixed evidence and limited guidance for the appropriate and meaningful selection of the appropriate approach for each encounter, and how to move towards integrated systems of care that weigh the appropriateness of care, and patient preference. In a report from 2021, Canadian Agency for Drugs and Technologies in Health (CADTH) conducted an informal jurisdictional scan on virtual care and suggested that effective virtual mental health care must include: 1) having an appropriate mix of modalities (e.g., phone, email) in delivering mental health care; 2) establishing a suitable payment model; 3) ensuring appropriate privacy and security safeguards are in place; 4) delivering quality patient care through and with the tool; and, 5) ensuring equitable delivery of virtual mental health care to marginalized populations.66
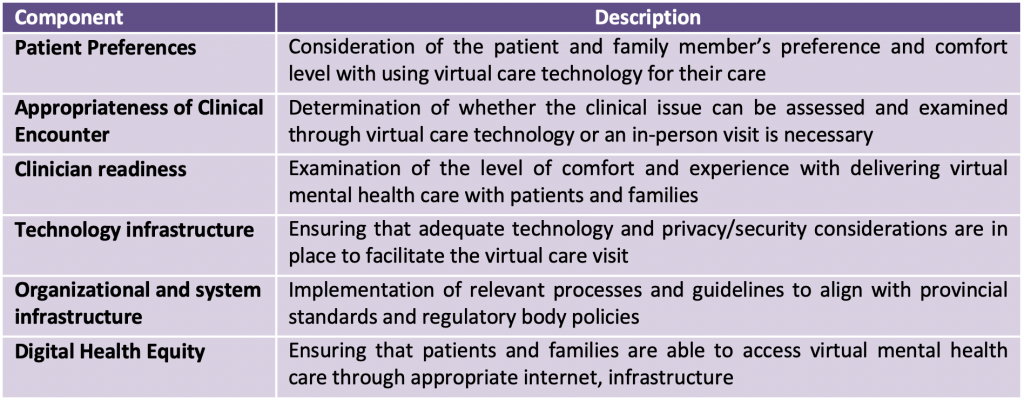
In this regard, several healthcare organizations have developed guidelines to help clinicians select the most appropriate modality for virtual health care. However, the efficacy of these guidelines has not been established. The University Health Network (UHN)67 in Toronto has suggested that clinicians should consider the clinical situation (e.g., procedures involved, objectives of the appointment) as well as patient preferences, access, and barriers in deciding whether to use virtual care. This should also extend to a discussion with the patient about their comfort level with technology, the need to include caregivers in the discussion, and the ability to access care on-site.67 Similarly, the South West Frail Senior Strategy Team in London, Ontario, co-created the ‘Virtual First Geriatric Model of Care’ with caregivers in the area.68 This model of care encourages clinicians to consider starting the clinical journey with a virtual consultation to determine the appropriate modality for the visit. In the initial consultation, the urgency of the situation, the patient’s needs, and access, as well as the type of subsequent consultation required can help inform the most appropriate modality for the visit.68 In this model of care, a checklist of ways to ensure a meaningful virtual encounter as well as approaches for conducting virtual cognitive assessments (e.g., MMSE, MoCAs) is also provided.68 Moreover, emerging frameworks such as the one from Heart & Stroke Foundation69 outline key considerations for successful implementation at both the user (e.g., readiness, issue at hand, appropriateness) and organizational level (e.g., system /environment, technology, clinical care).
While there have been no comprehensive guidelines specific to virtual mental health care to date, CAMH has developed some guidelines to help mental health care providers adhere to Ontario’s Privacy regulations in delivering virtual mental health care.70 This includes technology, security, and safety considerations, ways to confirm patient identity, as well as ensuring a private space for the individual to receive their care.70 A summary of some of the main components outlined from these frameworks can be found in Table 2.
Interpretation
With a significant increase in the number of virtual care visits and increased convenience and reach of virtual care for patients and families during the COVID-19 pandemic,14 it is likely that virtual delivery will remain a common modality for care delivery by mental healthcare professionals moving forward for mild to moderate mood and anxiety problems. With growing interest from organizations including the Canadian Medical Association12 and evidence on lessons learned and recommendations,71,72 it is expected that virtual mental health care will soon be used to support a broad range of mental health challenges in both primary and secondary care settings. However, there remains a lack of evidence on the efficacy of virtual mental health care for severe mental illness such as psychosis, in comparison to in-person care. As a result, until comparative evidence is available, it remains unclear what works best for who and traditional in-person options should continue to remain available.
Enabling the benefits and impact of virtual mental health care can only be realized when meaningful guidelines, training, and infrastructure (e.g., a balanced ‘mix’ with in-person services) is in place. For example, while the rapid adoption of virtual mental health care has led to numerous organizations developing guidance and policies around the safe and effective delivery of virtual mental health care, there is considerable variability in the guidelines, workflows, and processes across organizations. In particular, the lack of unified guidance and infrastructure at various organizations can create confusion and variable outcomes and experiences for patients and families.73 For example, while there is no accepted hierarchy across the various modalities, the lack of guidelines has led to differential remuneration across the use of in-person and virtual modalities. In Ontario, with in-person remuneration higher than virtual modalities, these approaches can lead to selection of modalities that is not based on evidence of effectiveness.74 In addition, the lack of guidelines can lead to cumbersome processes and documentation, which can generate patient safety concerns and contribute to unnecessary documentation burden on clinicians.75,76 These challenges can collectively lead to barriers and challenges for patients and families to access and use in an equitable manner. As such, based on the findings from the above, in this document, we make several recommendations to ensure that virtual mental health care in Ontario can be delivered in a manner that achieves the quadruple aim of health care, which encourages the delivery of care that enhances patient/clinician experience, quality of care and cost effectiveness.77
In addition, there is a strong need to examine the existing inequities of mental health care in the delivery of virtual care. Black and racialized populations have historically had disproportionate access to services, outcomes from mental health care and satisfaction with services.78 Given that Canada has a very diverse population, it is important to address the barriers that can perpetuate these inequities, such as language and use of interpreters. The Mental Health Commission of Canada has implemented a framework for examining inequities which comprise of three levels that are closely interconnected with each other: 1) system equity; 2) intervention equity; 3) equity in delivery of services. System equity focuses on access and outcomes and may include looking at service delivery models. Intervention equity looks at the effectiveness across diverse populations and this may include exploring the need for cultural adaptations of digital tools and services. Equity in delivering services includes the implementation and delivery aspects of the services and may include examining the capacity of therapists and their training/support for providing care to Black and racialized populations. To date, there is very limited work looking at the health equity considerations (e.g., training, support) required to implement sustainable, effective virtual mental health care for Canadians.
Future work should focus on research that expands our understanding of the effectiveness of virtual mental health care in large-scale, real-world settings, as well as implementation processes and the organizational and system-level factors that influence the delivery of virtual mental health care. Current documents have focused broadly on virtual care, and do not consider the specific nuances that are critical to consider for virtual mental health care (e.g., active suicidal ideation).79 Moreover, to date, only one study80 has focused on elucidating some of the system and organizational factors (e.g., workflow, setup support) that are relevant for facilitating and supporting virtual mental health care. With limited data on the organizational and system-level facilitators and barriers to delivering virtual mental health care, particularly to Black, racialized and/or marginalized populations, investing in projects that partner with racialized and underserved populations to examine system delivery of virtual care may be useful to better understand the challenges of accessing virtual mental health care at a population level.1 In addition, there is an absence of evidence around the differential efficacy and retention rates across the various virtual modalities of care (phone, video and in-person). Current data have highlighted that there is variability in the demographics81 and satisfaction82 in users of these modalities. It is likely that virtual interaction for mental health care may influence how individuals interact with the healthcare system. Thus, further research is needed to look at comparative effectiveness and acceptability of these modalities and to explore strategies to enhance delivery in a way that supports access and equity. Qualitative research83 can be a useful approach to help understand what patients and families envision in a mental health system that combines both in-person and virtual modalities. Lastly, it would be useful to examine how the delivery of virtual mental health care can be done to support the broader mental health care models such as measurement-based care, which involves the collection of questionnaires to assess patient symptoms and progression.84 Virtual delivery may offer additional opportunities to incorporate measurement-based care into routine mental health services, but feasible models that work for patients and providers will need to be developed and evaluated. Pre- and post-metrics may provide evidence of best practices. More importantly, given the team-based approach of mental health care services,22 it would be essential to look at this approach from various mental healthcare professionals, including physicians, nurses, case workers, social workers, psychotherapists and others. With most of the literature focused on physician use of virtual mental health care services,7 this can limit the ability to look at how other healthcare professionals involved in delivery of virtual mental health care can be best supported.
The following recommendations are guided by the existing evidence and best-practices described above:
1. Coordinate Local and Regional Planning of Virtual Care from a Health Systems Perspective
Planning and coordination of a sustainable, effective virtual mental health care strategy that complements the necessary in-person mental health services require consideration of the local and regional needs of the population and the health system. The delivery of virtual mental health care services using clinicians from their own regions and with insight from persons with lived experience in the community will allow for the delivery of care that fits within the local context and needs. Moreover, such an arrangement (as opposed to local hubs) can ensure flexible coordination of the program as the needs, resourcing, and demands of the community evolve over time.55 As such, the deployment of virtual mental health care programs should be done in close coordination with the available local and regional resources and funding.
2. Engage Individuals and Communities with Lived Experience in Virtual Mental Health Care Programs
Ensuring that the perspectives of patients, families and the community with lived experience in mental health challenges are represented in the decisions of health services delivery is essential for the delivery of care that meets the needs of end-users. Carmen et al. highlights numerous opportunities where patients and community stakeholders can participate in health systems planning.85 In this instance, forming a partnership or shared leadership with the local community in the development and implementation of processes and policies for virtual mental health care can help ensure that the decisions are made in close alignment with the needs of the community.
3. Develop Quality Standards for the Selection and Use of Virtual Mental Health Care
As outlined in the numerous virtual health toolkits from organizations across Ontario,67–69 there is a lack of standardization around the guidelines and recommendations for the selection and use of virtual mental health care. To ensure that the recommendations can deliver quality care to Ontarians, developing standards on the different modalities (i.e., telephone, in-person, video) would be useful given that each of these approaches can be appropriate for different populations and clinical situations. In addition, outlining the considerations for selecting the appropriate modality would help ensure that clinicians can confidently select the most appropriate to deliver care to patients. This is particularly important given that these decisions can impact treatment retention for different populations and communities (e.g., technology). While the current brief does not address the topic of remuneration, it would also be useful to examine how remuneration models and best practices align with the evidence and needs of patients and families. Lastly, among the different approaches, ensuring that appropriate privacy and security measures are in place is critical, given the sensitive nature of these discussions.86 Some individuals may not have access to the appropriate environment for a private conversation at home or in public spaces, and identifying opportunities with health systems and community organizations to provide these safe spaces may be warranted. Stigma may also be a key consideration. Thus, from an equity perspective, it would be useful to identify ways and interventions (e.g., offering services in multiple languages or with translation) that should be implemented in virtual mental health care services to support the inclusivity of diverse populations and needs.
4. Deliver Deliberate Guidance, Training, and Support on Virtual Mental Health Care for Patients, Families, and Healthcare Professionals
There is currently limited training and guidance that focuses on conducting therapeutic sessions over virtual modalities beyond the technical setup. With growing evidence of the use of virtual care for mental health assessment, treatment, and maintenance of the therapeutic relationship, there is a timely need to deliver training that fosters the core competencies required to successfully deliver virtual mental health care in a way that mirrors the delivery of quality in-person care.87,88 Based on the level of support, it would also be useful to look at the ability of clinicians to effectively triage patients to virtual and in-person modalities and their impact on treatment. Thus, developing curriculums and assessments that can be embedded into the training of current and future clinicians will be essential for equipping the workforce for a digitally-enabled mental health care environment. It is also important for administrators and clinicians to consider the origin of health disparities in the program planning and development process. The lack of appropriate consideration and acknowledgement of these disparities can perpetuate many of the ongoing disparities and the “digital divide”.89,90
5. Ensure Access to Necessary Infrastructure, Including Internet Connectivity for Black and Racialized Populations and Rural, Remote, and Northern Regions, Including First Nations Communities
While high-speed internet for virtual mental health care has become easily accessible in urban communities, it remains a significant challenge for many northern and rural communities. In a survey of high-speed internet availability reported by the Canadian Radio-television and Telecommunications Commission (CRTC), only 53% of households in rural areas have access to high-speed internet.91 Some regions also lack reliable electricity which is required for virtual visits with their mental health clinician.92 Moreover, with Canada being one of the most expensive countries for internet,93 affordability of high-speed internet continues to become a challenge for many marginalized groups including Black and racialized populations in urban settings. As a result, while virtual mental health care has a tremendous opportunity to support equity for people with mobility issues and anxiety (e.g., leaving home during the pandemic),29 ensuring affordable and accessible infrastructure is set up in these communities with an appropriate mix of in-person and virtual services is required for equitable delivery of virtual mental health care.
6. Consider the Diverse Needs, Preferences, and Values across Communities for Culturally Competent Virtual Mental Health Care
Given the diverse nature of the population of Ontario, delivering virtual mental health care requires consideration of the relevant needs, preferences, and values of specific communities, particularly among Black and racialized communities. The Digital Health Equity framework suggested that there is a need to consider the social and economic context (e.g., access to appropriate infrastructure, perceptions of using digital tools) in the equitable use of digital technologies.25 As such, understanding the language, values and living standards, as well as potential mental health stigma, will be important in ensuring appropriate setup and resources to deliver culturally-competent virtual mental health care in particular communities.
Methods Used for This Science Brief
A multi-pronged approach was used to rapidly identify evidence related to virtual mental health care. The Research, Analysis, and Evaluation Branch from the Ministry of Health synthesized information provided by the COVID-19 Evidence Synthesis Network members. Based on the feedback, the project team and the COVID-19 Mental Health Table provided additional comments and directions for policy recommendations. Relevant information identified in the screening of another literature review on virtual care (led by GS) was also added to inform this brief.
Based on the initial draft of the brief, numerous external members within the professional network of the project team were invited to comment and provide additional perspectives on the brief. This included administrators and clinicians with mental health organizations and mental health clinicians who provide care in rural communities outside the Greater Toronto Area. These individuals reviewed the drafts of this brief and provided their comments and recommendations back to the authors for inclusion, and we incorporated these perspectives throughout.
- Brewer LC, Fortuna KL, Jones C, et al. Back to the future: Achieving health equity through health informatics and digital health. JMIR MHealth UHealth. 2020;8(1):e14512. https://doi.org/10.2196/14512
- Beaunoyer E, Dupéré S, Guitton MJ. COVID-19 and digital inequalities: Reciprocal impacts and mitigation strategies. Comput Hum Behav.2020;111:106424. https://doi.org/10.1016/j.chb.2020.106424
- First Nations virtual doctor of the day brings culturally safe care to First Nations peoples across B.C. British Columbia Ministry of Health https://www2.gov.bc.ca/assets/gov/health/about-bc-s-health-care-system/heath-care-partners/health-newsletter/first-nation-doctor-summer-2021.pdf
- First Nations Health Authority. https://www.fnha.ca:443/what-we-do/ehealth/telehealth
- Kozelka EE, Jenkins JH, Carpenter-Song E. Advancing health equity in digital mental health: Lessons from medical anthropology for global mental health. JMIR Ment Health. 2021;8(8):e28555. https://doi.org/10.2196/28555
- Yellowlees P, Nakagawa K, Pakyurek M, Hanson A, Elder J, Kales HC. Rapid conversion of an outpatient psychiatric clinic to a 100% virtual telepsychiatry clinic in response to COVID-19. Psychiatr Serv. 2020;71(7):749-752. https://doi.org/10.1176/appi.ps.202000230
- Bhatia RS, Chu C, Pang A, Tadrous M, Stamenova V, Cram P. Virtual care use before and during the COVID-19 pandemic: A repeated cross-sectional study. Can Med Assoc Open Access J. 2021;9(1):E107-E114. https://doi.org/10.9778/cmajo.20200311
- Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ, Yellowlees PM. The effectiveness of telemental health: A 2013 review. Telemed E-Health. 2013;19(6):444-454. https://doi.org/10.1089/tmj.2013.0075
- Adopting and integrating virtual visits into care: Draft clinical guidance. Ontario Health; 2020:27. https://quorum.hqontario.ca/Portals/0/Users/170/54/10154/Draft%20Clinical%20Guidance_Adopting%20and%20integrating%20virtual%20visits%20into%20care_V1.pdf?ver=2020-03-13-091936-370
- E-mental health in Canada: Transforming the mental health system using technology. Mental Health Commision of Canada; 2014. https://www.mentalhealthcommission.ca/wp-content/uploads/drupal/MHCC_E-Mental_Health-Briefing_Document_ENG_0.pdf
- E-mental health demonstration project. Mental Health Commision of Canada; 2019. https://www.mentalhealthcommission.ca/wp-content/uploads/drupal/2019-09/emental_health_report_eng_0.pdf
- Smith A. Virtual care playbook. The College of Family Physicians of Canada; 2021:16. https://www.cma.ca/sites/default/files/pdf/Virtual-Care-Playbook_mar2020_E.pdf
- Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021;193(6):E200-E210. https://doi.org/10.1503/cmaj.202303
- Mental health in canada: COVID-19 and beyond. Centre for Addiction and Mental Health; 2020. https://www.camh.ca/500.html?aspxerrorpath=/en/health-info/mental-health-and-covid-19
- Schwamm LH, Estrada J, Erskine A, Licurse A. Virtual care: New models of caring for our patients and workforce. Lancet Digit Health. 2020;2(6):e282-e285. https://doi.org/10.1016/S2589-7500(20)30104-7
- Anderson J, Ganguli I. Unpacking the potential for virtual care. J Gen Intern Med. 2019;34(12):2906-2907. https://doi.org/10.1007/s11606-019-05201-5
- Spelman JF, Brienza R, Walsh RF, et al. A model for rapid transition to virtual care, VA connecticut primary care response to COVID-19. J Gen Intern Med. 2020;35(10):3073-3076. https://doi.org/10.1007/s11606-020-06041-4
- Curfman A, Zuckerman A, Wilson A, et al. vKids at home: In-home virtual care for complex pediatric patients. Pediatrics. 2021. https://doi.org/10.1542/peds.147.3MA10.992a
- Hogan J, Boykin D, Schneck CD, et al. Clinical lessons from virtual house calls in mental health: The doctor is in the house. Psychiatr Clin North Am. 2019;42(4):575-586. https://doi.org/10.1016/j.psc.2019.08.004
- Ben-Zeev D. The digital mental health genie is out of the bottle. Psychiatr Serv. 2020;71(12):1212-1213. https://doi.org/10.1176/appi.ps.202000306
- Bower P, Gilbody S. Stepped care in psychological therapies: Access, effectiveness and efficiency: Narrative literature review. Br J Psychiatry. 2005;186(1):11-17. https://doi.org/10.1192/bjp.186.1.11
- Katzelnick DJ, Williams MD. Large-scale dissemination of collaborative care and implications for psychiatry. Psychiatr Serv. 2015;66(9):904-906. https://doi.org/10.1176/appi.ps.201400529
- Boudreau DM, Capoccia KL, Sullivan SD, et al. Collaborative care model to improve outcomes in major depression. Ann Pharmacother. 2002;36(4):585-591. https://doi.org/10.1345/aph.1A259
- Kemp J, Zhang T, Inglis F, et al. Delivery of compassionate mental health care in a digital technology–driven age: Scoping review. J Med Internet Res. 2020;22(3):e16263. https://doi.org/10.2196/16263
- Crawford A, Serhal E. Digital health equity and COVID-19: The innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020;22(6):e19361. https://doi.org/10.2196/19361
- Stamenova V, Chu C, Pang A, Tadrous M, Bhatia RS, Cram P. Using administrative data to explore potentially aberrant provision of virtual care during COVID-19: Retrospective cohort study of ontario provincial data. J Med Internet Res. 2021;23(9):e29396. https://doi.org/10.2196/29396
- Canadians’ health care experiences during COVID-19: Uptake of virtual care. Canada Health Infoway; 2022. https://www.infoway-inforoute.ca/en/component/edocman/3828-canadians-health-care-experiences-during-covid-19/view-document?Itemid=0_
- Virtual care in Canada. Canadian Institute for Health Information. Published April 2022. https://www.cihi.ca/en/virtual-care-in-canada
- Wong A, Bhyat R, Srivastava S, Boissé Lomax L, Appireddy R. Patient care during the COVID-19 pandemic: Use of virtual care. J Med Internet Res. 2021;23(1):e20621. https://doi.org/10.2196/20621
- Assessing the effectiveness of virtual care for adults with mental health and/or addictions issues. McMaster University; 2020:36. https://covid19mentalhealthresearch.ca/wp-content/uploads/2021/01/LAVIS-rr_covid-19_assessing-the-effectiveness-of-virtual-care-for-adults-with-mental-health-and-or-addictions-issues.pdf
- Drago A, Winding TN, Antypa N. Videoconferencing in psychiatry, a meta-analysis of assessment and treatment. Eur Psychiatry. 2016;36:29-37. https://doi.org/10.1016/j.eurpsy.2016.03.007
- Watt JA, Lane NE, Veroniki AA, et al. Diagnostic accuracy of virtual cognitive assessment and testing: Systematic review and meta-analysis. J Am Geriatr Soc. 2021;69(6):1429-1440. https://doi.org/10.1111/jgs.17190
- Dellazizzo L, Léveillé N, Landry C, Dumais A. Systematic review on the mental health and treatment impacts of COVID-19 on neurocognitive disorders. J Pers Med. 2021;11(8):746. https://doi.org/10.3390/jpm11080746
- Lavigne KM, Sauvé G, Raucher-Chéné D, et al. Remote cognitive assessment in severe mental illness: A scoping review. Schizophrenia. 2022;8(1):1-12. https://doi.org/10.1038/s41537-022-00219-x
- Lawes-Wickwar S, McBain H, Mulligan K. Application and effectiveness of telehealth to support severe mental illness management: Systematic review. JMIR Ment Health. 2018;5(4):e8816. https://doi.org/10.2196/mental.8816
- Best MW. CIHR knowledge synthesis: Examining the efficacy of evidence-based psychosocial interventions for schizophrenia-spectrum disorders delivered through virtual care. TIP Research Lab; 2020:29. https://irsc-cihr.gc.ca/e/documents/Best-Initial-Knowledge-Synthesis-2020-06-22.pdf
- Firth J, Cotter J, Torous J, Bucci S, Firth JA, Yung AR. Mobile phone ownership and endorsement of “mHealth” among people with psychosis: A meta-analysis of cross-sectional studies. Schizophr Bull. 2016;42(2):448-455. https://doi.org/10.1093/schbul/sbv132
- Berry N, Lobban F, Emsley R, Bucci S. Acceptability of interventions delivered online and through mobile phones for people who experience severe mental health problems: A systematic review. J Med Internet Res. 2016;18(5):e5250. https://doi.org/10.2196/jmir.5250
- Gagnon M, Chouinard M. Digital health interventions for the prevention, detection and management of mental health problems in people with chronic diseases in times of COVID-19: An overview. Canadian Institutes of Health Research; 2020:69. http://www.uqac.ca/portfolio/maximesasseville/files/2019/03/Synth%C3%A8se-IRSC-23-novembre_mpg_MS.pdf
- Coughtrey AE, Pistrang N. The effectiveness of telephone-delivered psychological therapies for depression and anxiety: A systematic review. J Telemed Telecare. 2018;24(2):65-74.https://doi.org/10.1177/1357633X16686547
- Yellowlees P, Richard Chan S, Burke Parish M. The hybrid doctor–patient relationship in the age of technology: Telepsychiatry consultations and the use of virtual space. Int Rev Psychiatry. 2015;27(6):476-489. https://doi.org/10.3109/09540261.2015.1082987
- “I’m not feeling like i’m part of the conversation” patients’ perspectives on communicating in clinical video telehealth visits. Springer Link. Published online February 2020. https://link.springer.com/article/10.1007/s11606-020-05673-w
- Tzelepis F, Paul CL, Williams CM, et al. Real‐time video counselling for smoking cessation. Cochrane Database Syst Rev. 2019;(10). https://doi.org/10.1002/14651858.CD012659.pub2
- Sachs JW, Graven P, Gold JA, Kassakian SZ. Disparities in telephone and video telehealth engagement during the COVID-19 pandemic. JAMIA Open. 2021;4(3):ooab056. https://doi.org/10.1093/jamiaopen/ooab056
- Missiuna S, Plante C, Pahwa P, Muhajarine N, Neudorf C. Trends in mental health inequalities in urban Canada. Can J Public Health Rev Can Santé Publique. 2021;112(4):629-637. https://doi.org/10.17269/s41997-021-00498-4
- Ross LE, Gibson MF, Daley A, Steele LS, Williams CC. In spite of the system: A qualitatively-driven mixed methods analysis of the mental health services experiences of LGBTQ people living in poverty in Ontario, Canada. PLoS ONE. 2018;13(8):e0201437. https://doi.org/10.1371/journal.pone.0201437
- Public Health Agency of Canada. Infographic: Inequalities in mental illness hospitalization in Canada. Published April 24, 2019. https://www.canada.ca/en/public-health/services/publications/science-research-data/inequalities-mental-illness-hospitalization-infographic.html
- Urbanoski K, Inglis D, Veldhuizen S. Service use and unmet needs for substance use and mental disorders in Canada. Can J Psychiatry Rev Can Psychiatr. 2017;62(8):551-559. https://doi.org/10.1177/0706743717714467
- Ghidei W, Montesanti S, Tomkow K, Silverstone PH, Wells L, Campbell S. Examining the effectiveness, acceptability, and feasibility of virtually delivered trauma-focused domestic violence and sexual violence interventions: A rapid evidence assessment. Trauma Violence Abuse. Published online March 27, 2022:15248380211069060. https://doi.org/10.1177/15248380211069059
- Thomeer MB, Moody MD, Yahirun J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J Racial Ethn Health Disparities. Published online March 22, 2022. https://doi.org/10.1007/s40615-022-01284-9
- Sanford S, Um S gee, Tolentino M, et al. The impact of COVID-19 on mental health and well-being: A focus on racialized communities in the GTA. Wellsley Institute; 2022:44. https://www.wellesleyinstitute.com/wp-content/uploads/2022/03/The-Impact-of-COVID-19-on-Mental-Health-and-Well-being-A-Focus-on-Racialized-Communities-in-the-GTA.pdf
- Andrey S, Dorkenoo S, Malli N, Masoodi M (Joe). Mapping Toronto’s digital divide. Brookfield Institute for Innovation + Entrepreneurship; 2021. https://brookfieldinstitute.ca/mapping-torontos-digital-divide
- Caxaj CS. A review of mental health approaches for rural communities: Complexities and opportunities in the Canadian context. Can J Commun Ment Health. 2016;35(1):29-45. https://doi.org/10.7870/cjcmh-2015-023
- Lambert D, Gale J, Hartley D, Croll Z, Hansen A. Understanding the business case for telemental health in rural communities. J Behav Health Serv Res. 2016;43(3):366-379. https://doi.org/10.1007/s11414-015-9490-7
- Fortney JC, Pyne JM, Turner EE, et al. Telepsychiatry integration of mental health services into rural primary care settings. Int Rev Psychiatry. 2015;27(6):525-539. https://doi.org/10.3109/09540261.2015.1085838
- Harerimana B, Forchuk C, O’Regan T. The use of technology for mental healthcare delivery among older adults with depressive symptoms: A systematic literature review. Int J Ment Health Nurs. 2019;28(3):657-670. https://doi.org/10.1111/inm.12571
- Serhal E, Lazor T, Kurdyak P, et al. A cost analysis comparing telepsychiatry to in-person psychiatric outreach and patient travel reimbursement in Northern Ontario communities. J Telemed Telecare. 2020;26(10):607-618. https://doi.org/10.1177/1357633X19853139
- Serhal E, Iwajomo T, de Oliveira C, Crawford A, Kurdyak P. Characterizing family physicians who refer to telepsychiatry in Ontario. Can J Psychiatry. 2021;66(1):25-33. https://doi.org/10.1177/0706743720954061
- Strudwick G, Sockalingam S, Kassam I, et al. Digital interventions to support population mental health in Canada during the COVID-19 pandemic: Rapid review. JMIR Ment Health. 2021;8(3). https://doi.org/10.2196/26550
- Camp P, Girt M, Wells A, et al. Virtual care for indigenous populations in Canada, the United States, Australia, and New Zealand: Protocol for a scoping review. JMIR Res Protoc. 2020;9(12):e21860. https://doi.org/10.2196/21860
- Toombs E, Kowatch KR, Dalicandro L, McConkey S, Hopkins C, Mushquash CJ. A systematic review of electronic mental health interventions for Indigenous youth: Results and recommendations. J Telemed Telecare. 2021;27(9):539-552. https://doi.org/10.1177/1357633X19899231
- Hensel JM, Ellard K, Koltek M, Wilson G, Sareen J. Digital health solutions for Indigenous mental well-being. Curr Psychiatry Rep. 2019;21(8):68. https://doi.org/10.1007/s11920-019-1056-6
- Statistics Canada Government of Canada. Results from the 2016 Census: Housing, income and residential dissimilarity among Indigenous people in Canadian cities. Published December 10, 2019. https://www150.statcan.gc.ca/n1/pub/75-006-x/2019001/article/00018-eng.htm
- Canadian Institutes of Health Research Government of Canada. Niikaniganaw (all my relations) ii – the COVID-19 rapid response: Indigenous approaches to synthesizing knowledge for culturally-safe and stigma free mental health care for under-served indigenous communities in Ottawa-Gatineau. Published June 17, 2020. https://cihr-irsc.gc.ca/e/52037.html
- Canadian Institutes of Health Research Government of Canada. Dr. Michaela Hynie: Promising practices in helping refugees access virtual mental health services during COVID-19. Published April 20, 2022. https://cihr-irsc.gc.ca/e/52928.html
- Gray C, Mason J, Loshak H. An overview of direct-to-patient virtual visits in Canada. Canadian Agency for Drugs and Technologies in Health; 2021. http://canjhealthtechnol.ca/index.php/cjht/article/view/eh0091
- Clinical guiding principles for virtual care. UHN; 2022:5. https://www.uhn.ca/corporate/AboutUHN/Virtual_Care/Documents/Clinical-Guiding-Principles-Virtual-Care.pdf
- Providing geriatric virtual care across the South West: Guidance document for health care and community support services providers. South West Frail Senior Strategy’s (SWFSS); 2020. https://www.sjhc.london.on.ca/media/8411/download
- Virtual care decision framework. Heart and Stroke Foundation; 2021. https://heartstrokeprod.azureedge.net/-/media/1-stroke-best-practices/csbp-f20-virtualcaredecisionframework-en.ashx?la=en&rev=9db7990386364a1b8253401c0313d634
- Telemental health – portico network. https://www.porticonetwork.ca/web/telemental-health
- Gratzer D, Torous J, Lam RW, et al. Our digital moment: Innovations and opportunities in digital mental health care. Can J Psychiatry. 2021;66(1):5-8. https://doi.org/10.1177/0706743720937833
- Hawke LD, Sheikhan NY, MacCon K, Henderson J. Going virtual: youth attitudes toward and experiences of virtual mental health and substance use services during the COVID-19 pandemic. BMC Health Serv Res. 2021;21(1):340. https://doi.org/10.1186/s12913-021-06321-7
- Herzer KR, Pronovost PJ. Ensuring quality in the era of virtual care. JAMA. 2021;325(5):429-430. https://doi.org/10.1001/jama.2020.24955
- Ontario’s doctors ratify new three-year agreement with province. Ontario Medical Association. Published May 2022. https://www.oma.org/newsroom/news/2022/march/ontarios-doctors-ratify-new-three-year-agreement-with-province/
- Engineering National Academies of Sciences. Taking action against clinician burnout: A systems approach to professional well-being. https://doi.org/10.17226/25521
- Ontario Medical Association. Healing the Healers: System-Level Solutions to Physician Burnout. Ontario Medical Association; 2021:48. https://www.oma.org/uploadedfiles/oma/media/pagetree/advocacy/health-policy-recommendations/burnout-paper.pdf
- Bodenheimer T, Sinsky C. From triple to quadruple aim: Care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. https://doi.org/10.1370/afm.1713
- Deferio JJ, Breitinger S, Khullar D, Sheth A, Pathak J. Social determinants of health in mental health care and research: A case for greater inclusion. J Am Med Inform Assoc. 2019;26(8-9):895-899.https://doi.org/10.1093/jamia/ocz049
- Simon GE, Stewart CC, Gary MC, Richards JE. Detecting and assessing suicide ideation during the COVID-19 pandemic. Jt Comm J Qual Patient Saf.2021;47(7):452-457. https://doi.org/10.1016/j.jcjq.2021.04.002
- Budhwani S, Fujioka JK, Chu C, et al. Delivering mental health care virtually during the COVID-19 pandemic: Qualitative evaluation of provider experiences in a scaled context. JMIR Form Res. 2021;5(9):e30280. https://doi.org/10.2196/30280
- Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(1):21-26.https://doi.org/10.37765/ajmc.2021.88573
- Donelan K, Barreto EA, Sossong S, et al. Patient and clinician experiences with telehealth for patient follow-up care. Am J Manag Care. 2019;25(1):40-44. https://pubmed.ncbi.nlm.nih.gov/30667610/
- Qualitative Research&evaluation Methods. Sage Publishing; 2022. https://us.sagepub.com/en-us/nam/qualitative-research-evaluation-methods/book232962
- Lewis CC, Boyd M, Puspitasari A. Implementing measurement-based care in behavioral health: A review. JAMA Psychiatry. Published online 2018. https://jamanetwork.com/journals/jamapsychiatry/article-abstract/2718629
- Carman KL, Dardess P, Maurer M, et al. Patient and family engagement: A framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). 2013;32(2):223-231. https://doi.org/10.1377/hlthaff.2012.1133
- Levy S, Deister D, Fantegrossi J, et al. Virtual care in an outpatient subspecialty substance use disorder treatment program. J Addict Med. 2022;16(2):e112. https://doi.org/10.1097/ADM.0000000000000871
- Bolster MB, Chandra S, Demaerschalk BM, et al. Crossing the virtual chasm: Practical considerations for rethinking curriculum, competency, and culture in the virtual care era. Acad Med. 2022;97(6):839-846.https://doi.org/10.1097/ACM.0000000000004660
- Sharma R, Nachum S, Davidson KW, Nochomovitz M. It’s not just FaceTime: core competencies for the Medical Virtualist. Int J Emerg Med. 2019;12(1):8. https://doi.org/10.1186/s12245-019-0226-y
- Veinot TC, Mitchell H, Ancker JS. Good intentions are not enough: How informatics interventions can worsen inequality. J Am Med Inform Assoc. 2018;25(8):1080-1088. https://doi.org/10.1093/jamia/ocy052
- WHO Global Observatory for eHealth. MHealth: New Horizons for Health through Mobile Technologies: Second Global Survey on EHealth. World Health Organization; 2011. https://apps.who.int/iris/handle/10665/44607
- Canadian Radio-television and Telecommunications Commission (CRTC) Government of Canada. Broadband fund: Closing the digital divide in Canada. Published January 14, 2016. https://crtc.gc.ca/eng/internet/internet.htm
- Status of Remote/off-Grid Communities in Canada. Government of Canada; 2011. https://www.nrcan.gc.ca/sites/www.nrcan.gc.ca/files/canmetenergy/files/pubs/2013-118_en.pdf
- Canada’s internet prices are rising again — and critics say the CRTC’s broadband reversal is to blame. thestar.com. Published July 20, 2022. https://www.thestar.com/business/2022/07/20/canadas-internet-prices-now-highest-in-the-world-for-some-speeds-continue-to-climb-report-finds.html
Author Contributions: BO, GS, BL, LM and CM conceived of the Science Brief. BL, GS and BO wrote the first draft of the Science Brief. BL, BO and GS led subsequent revisions to the Science Brief. All authors revised the Science Brief for critically important intellectual content and approved the final version.
The authors would like to thank Kwame McKenzie for his comments and review of this Science Brief.
Citation: Lo B, Strudwick G, Mah L, et al. Effective modalities of virtual care to deliver mental health and addictions services in Canada. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2022;3(66). https://doi.org/10.47326/ocsat.2022.03.66.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
