Impact of Hospital Visitor Restrictions during the COVID-19 Pandemic
Authors:Laveena Munshi, Ayodele Odutayo, Gerald A. Evans, Maggie Keresteci, Julie Drury, Dylan Kain, Jennie Johnstone, Nathan M. Stall, Kali Barrett, Arthur S. Slutsky, Antonina Maltsev, Anna Perkhun, Peter Jüni, Fahad Razak on behalf of the Ontario COVID-19 Science Advisory Table
Key Message
The rationale for restrictive “no visitor” policies adopted during the first wave of the COVID-19 pandemic was to limit the introduction of SARS-CoV-2 into the hospitals and to minimize the risk of transmission to the community. Available research demonstrates that (1) general hospital visitors need to be distinguished from “family/essential caregivers”, (2) family/essential caregivers do not play a substantial role in the transmission of SARS-CoV-2 in a hospital setting with infection and prevention control (IPAC) measures, and (3) blanket restrictive visitor policies are associated with potential harms particularly across specific populations.
Visitor policies which are typically established locally by each hospital must balance the potential infection risk associated with having family/essential caregivers in the hospital against the risk to specific patient populations and the resultant increase in workload to health care providers in the absence of family/essential caregivers. While creative electronic mechanisms to enhance communication between patients, their families, and the health care team were rapidly adopted, more research is needed to ensure these adaptations are culturally appropriate and equitable.
Summary
Background
Restrictive “no visitor” policies were adopted during the first wave of the COVID-19 pandemic in an attempt to mitigate SARS-CoV-2 transmission from the community to health care workers and patients, protect visitors from acquiring SARS-CoV-2, and to preserve limited supplies of personal protective equipment (PPE).
Questions
What was the public health-related rationale behind strict visitor policies?
What are the benefits to patients, families, and health care providers from family/essential caregivers, and what are the harms associated with restrictive visitor policies?
How can we safely introduce family/essential caregivers to the bedside?
What mechanisms exist to mitigate harms associated with family/essential caregiver absence and strict visitor policies?
Findings
It is imperative that visitor policies clearly distinguish general “hospital visitors” from “family/essential caregivers”. Family/essential caregivers encompass family and/or friend caregivers designated by the patient who provide important essential care and support to patients admitted to hospital. When referring to visitors in this brief, we consider only the role of family/essential caregivers.
Available research suggests that family/essential caregivers do not play a substantial role in the transmission of SARS-CoV-2. Furthermore, an extensive body of literature demonstrates that family/essential caregivers are important in the delivery of patient-centred care. This includes: assisting with patient advocacy, feeding, mobility, orientation (delirium/cognitive impairment), communication in the setting of language barriers, during labour and delivery, during transitions in care, including to critical care, and support at the end of life.
Blanket restrictive visitor policies are associated with potential harm across these populations, interrupt the natural exchange of information between the health care team and the patient’s family/essential caregiver, are associated with complicated grief across family members at the end-of-life, and may contribute to moral distress among clinicians.
Most jurisdictions used technology such as video calls or teleconferences to facilitate communication between patients, health care teams, and families. This was found to be feasible and acceptable across the studies that assessed these types of communication. However, there were some common challenges faced: (1) a lack of familiarity with technology, (2) nursing time constraints, (3) privacy considerations, and (4) equitable access to devices.
Interpretation
There remain specific circumstances (e.g., hospital outbreaks) where strict visitor policies may be required; however, exceptions need to be made for essential caregivers to assist with the provision of care. The degree of restriction established by the hospitals must balance infection risk against the risk to specific patient populations and the resultant increase in workload to health care providers in their absence. Appropriate access and training in IPAC can facilitate the safe introduction of family/essential caregivers. Furthermore, vaccination against SARS-CoV-2 offers family/essential caregivers further protection and reduces their risk, particularly with ongoing IPAC measures. Mechanisms to appeal restrictions must be transparent, accessible, and timely. Family/essential caregivers should be involved in the development of future visiting policies where distinctions are made between essential caregivers and general social visitors.
Existing literature does not support any scenario where a complete restriction of family/essential caregivers across all patient subtypes from hospitals is required. Many institutions in Canada have adopted less restrictive policies in specific settings, recognizing the importance of family/essential caregivers in the second and third wave of the pandemic after reflecting upon their experience in the first wave.
Full text
Background
The COVID-19 pandemic, caused by SARS-CoV-2, continues to place significant strain on health care systems worldwide. At the onset of the pandemic, an almost complete restriction of visitors occurred across all hospitals surveyed in a 35-hospital pan-Canadian study.2 The data in support of these restrictions was largely extrapolated from studies surrounding mechanisms of transmission, knowledge from prior pandemics, and concerns around PPE supply. The action was an application of the ‘precautionary principle’, a core recommendation in the 2007 SARS Commission report.3 These policies sought to balance the interests of the individual patient against our utilitarian responsibility as a society to mitigate the transmission to, from, and within hospitals.
It is essential to note that hospital visitors range from individuals who are visiting for social reasons to essential caregivers. Essential caregivers are individuals (family or friends) who are active and essential in the ongoing care of a patient admitted to the hospital. For the purpose of this Science Brief, the term “visitor” excludes social visits and refers specifically to family or friends, designated by the patient, who act as essential caregivers. These individuals will be referred to as family/essential caregivers throughout this brief.
Questions
What was the public health-related rationale behind strict visitor policies?
What are the benefits to patients, families, and health care providers from family/essential caregivers, and what are the harms associated with restrictive visitor policies?
How can we safely introduce family/essential caregivers to the bedside?
What mechanisms exist to mitigate harms associated with family/essential caregiver absence and strict visitor policies?
Findings
Public Health-Related Rationale for Strict Visitor Policies
Strict policies restricting hospital visitors had a number of aims: (1) to prevent the transmission of COVID-19 from the community to the healthcare setting (infecting health care workers and patients), (2) to prevent transmission from the healthcare setting to the community (infecting visitors), and (3) to preserve PPE when concerns existed surrounding supplies. At the onset of the pandemic, the potential of visitor-related COVID-19 outbreaks was considered to be a sufficient risk. As such, all types of visitors were restricted, despite a lack of scientific evidence linking visitors to SARS-CoV-2 transmission. Furthermore, in very overwhelmed health care systems internationally with high volumes of patients, it was believed that these restrictions would allow more control over the environment in an attempt to minimize transmission.
Historical Perspective
Outside of pandemics, restrictive visitor policies across hospitals were built on historical roots extending from the 1800s. There existed a belief in medicine that a liberal approach to visiting would be associated with increased physiologic stress, physical and emotional “exhaustion” for patients, and impair the provision of care by health care workers. However contemporary data from the inpatient and critical care settings has demonstrated that these concerns are not grounded in evidence.
Emerging evidence over the past two decades has shown a clear benefit of family/essential caregiver presence across patient populations.4–8 In response to this, a gradual relaxation of visitor restrictions has been seen over the decades. By early 2020, just prior to the COVID-19 pandemic, a review of hospitals by the Canadian Foundation for Healthcare Improvement found that 73% of hospitals had adopted accommodating visitor policies (increased from 32% in 2015).9
COVID-19
A limited number of studies have evaluated the potential risk posed by family/essential caregivers during the COVID-19 pandemic. Studies evaluating asymptomatic prevalence of COVID-19 among family/essential caregivers who had screened negative for symptoms ranged from 4 to 10% in studies from Brazil and New York.10,11 However, this data was obtained during periods of high community prevalence of SARS-CoV-2 and prior to the adoption of public masking in New York. Furthermore, given the lack of access to testing for the general public early in the pandemic, it is possible that many individuals that tested positive had old infections, and were no longer communicable, despite positive RT-PCR testing. Data from asymptomatic serial screening of unvaccinated long-term care (LTC) staff in Ontario revealed low rates of positive results (<0.4%), even during periods where prevalence was high.12
Published studies from the first wave of the pandemic demonstrate that the risk posed by family/essential caregivers is low. Early in the pandemic, prior to the widespread implementation of public health and IPAC measures, a systematic review of nosocomial acquisition of SARS-CoV-2 from case series in Wuhan, China demonstrated that 2% of nosocomial acquired cases were from visitors.13 These occurred during a time of insufficient protective measures for patients, health care workers and visitors (e.g., sufficient personal protective measures).
A subsequent study conducted in the United States between March 7 and May 30, 2020, of 9,149 hospitalized patients found low rates of hospital-acquired SARS-CoV-2.14 Only one of the 12 cases diagnosed among patients after three days in hospital was deemed to be acquired from a pre-symptomatic family/essential caregiver before restrictions were implemented. The low rates cannot be attributable solely to visitor restrictions as policies and universal masking of family/essential caregivers were implemented at the midpoint of this study time-period (April 3 and April 6, 2020, respectively).
In a study from a tertiary care hospital in Singapore, nosocomial-associated respiratory viral infections were tracked from June to August 2020 as visitor policies relaxed, with sufficient IPAC measures in place – including universal masking – from no family/essential caregivers, to one, and then two family/essential caregivers.15 There was no statistically significant difference in nosocomial associated respiratory viral infections when they relaxed their policy to one or two family/essential caregivers per day, compared to no family/essential caregivers. Outside of the COVID-19 pandemic, a systematic review evaluating liberal versus restrictive policies in a critical care setting found no increase in acquired infections with liberal visitor policies.16 A more detailed description of these studies is available in Appendix A.
How the risk profile of family/essential caregivers changes as the community incidence of SARS-CoV-2 changes or community vaccination rates increase remains unknown. We presume that as case counts drop and the community is increasingly vaccinated, the risk posed is further reduced. However, the risk of family/essential caregivers since the emergence of highly transmissible variants of concern (VOCs), including B.1.1.7, is not known.
Important factors that may contribute to visitors representing a higher risk to healthcare settings include higher prevalence of the virus in the community, low vaccination status, the presence of more transmissible VOCs – particularly when there is uncertainty about their susceptibility to the current vaccines and inconsistent PPE use (especially universal masking around loved ones).
Other factors that may influence risk include asymptomatic carriers and a lack of recognition of symptoms or exposures by a visitor. Family/essential caregivers are likely to represent less risk to healthcare settings when there is lower community incidence of SARS-CoV-2, when family/essential caregivers are vaccinated, and when family/essential caregivers are provided with training on IPAC policies and use of PPE. This includes consistent use of masking around their loved ones and designated separate spaces for eating and drinking. Vaccination status against SARS-CoV-2 (1 or 2 doses) likely further protects the family/essential caregiver and reduces the risk of family/essential caregivers in the hospital setting with ongoing IPAC measures.
Benefits to Patients, Families, and Health Care Providers from Family/Essential Caregivers, and the Harms Associated with Restrictive Visitor Policies
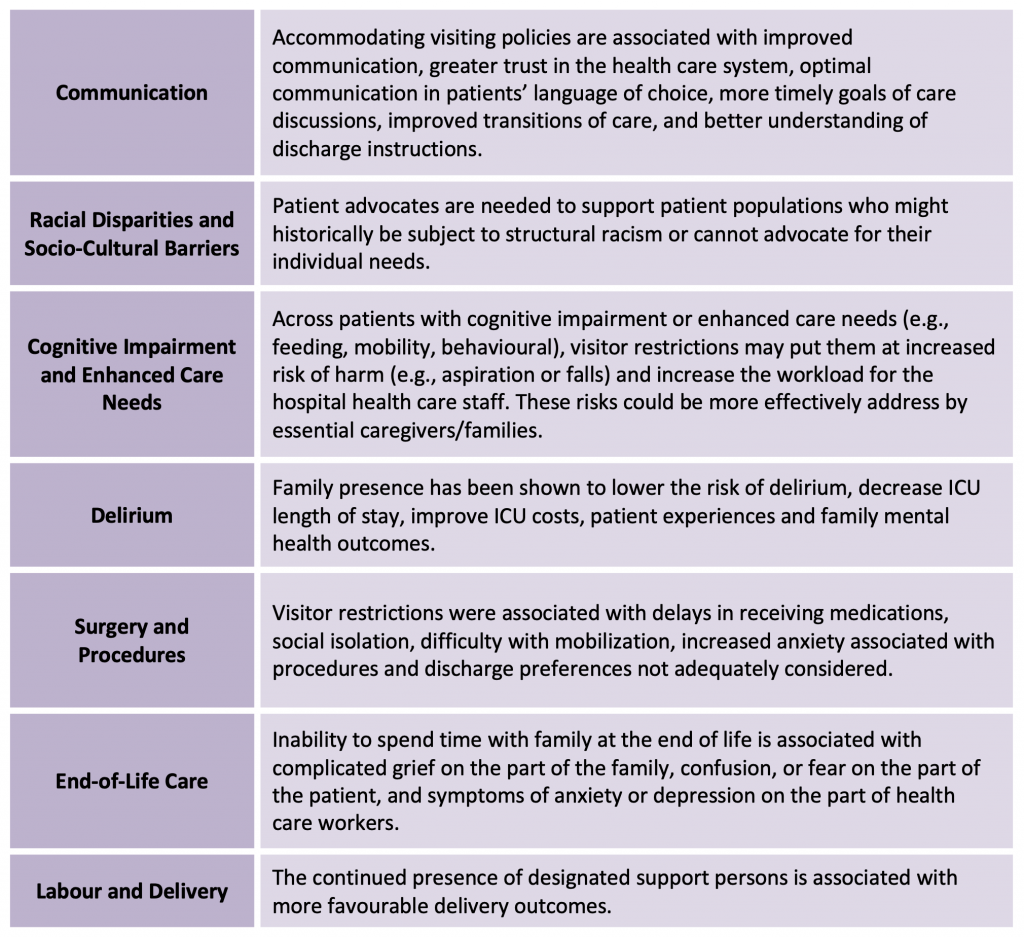
Previous literature has demonstrated that family/essential caregiver presence is associated with benefits to patient care including improved safety, enhanced communication and improved outcomes.1,17–22 Family/essential caregivers are also crucial players in the delivery of patient-centred care by assisting with feeding, mobility, hygiene, orientation, and emotional support (Table 1).
Communication and Advocacy
Visitor policies that accommodate caregivers have been shown to improve communication and build trust between families and care providers. They further improve the accuracy and quality of information surrounding a diagnosis, transitions of care, and discharge instructions. Language barriers are common in Canada and lead to poorer quality health care. Language barriers can be misclassified as delirium, leading to unnecessary and inappropriate use of psychotropic medications or physical restraints for hyperactive delirium.23 In the pediatric literature, family presence has been found to improve hospital safety through increased surveillance and detection of potential medical errors.24 When patients experience a change in their clinical status or clinical condition that prevents them from articulating their preferences, family members and substitute decision makers become essential in communication surrounding escalation of care, particularly in the setting of incapacity.4
Visitor restrictions have disrupted the routine structure and processes of family communication and in-person meetings.5 A study carried out during the COVID-19 pandemic by Piscitello and colleagues evaluated the content of family meetings which used electronic communication for critically ill patients who lacked decision making capacity. Goals of care re-evaluations and modifications were less likely to occur over video communication compared to in-person meetings (11% vs. 35%, p=0.0006).25 Challenges in the exchange of information and timely involvement in decision-making have been further compounded by unprecedented increases in clinical demands in the general internal medicine and intensive care unit (ICU) settings. All of these factors limit timely and effective communication with families.
Racial disparities and structural racism have been documented across the provision of health care. Pandemics amplify underlying pre-existing health disparities.44 Patient advocacy has been one mechanism to mitigate the potential for structural racism in health care. Visitor restrictions limit the presence of family/essential caregivers who may act as patient advocates for more vulnerable patients who might historically have been subject to structural racism. These restrictions could pose a disproportionate risk to this population. More data is needed to evaluate the impact of visitor restrictions in this population.6,7
Delirium
Patients with COVID-19 critical illness experience a high incidence of acute brain dysfunction and delirium.26–28 In general, patients with delirium have longer hospital stays and are at increased risk of ICU mortality.29,30 In a study evaluating 2,088 critically ill COVID-19 patients, 55% (1,147 patients) were delirious for a median of 3 days (interquartile range (IQR) 2 to 6).31 Across this cohort of patients with COVID-19, visits by family/essential caregivers (in person or virtual) have been shown to reduce the odds of delirium (Odds Ratio (OR) 0.73, 95% confidence interval (CI) 0.63 to 0.84, p<0.0001).27 Outside of COVID-19, family-centered care interventions have demonstrated a decreased ICU length of stay in a meta-analysis, by a mean of 1.21 days (95% CI, 2.25 to 0.16, I2: 26%).8 Family-centred interventions also improved ICU costs, patient experience and patient/family mental health.8
Surgery
Zeh and colleagues evaluated 117 patients without COVID-19 who underwent surgery from February to April, 2020.32Those exposed to visitor restrictions had delays in receiving medications, greater social isolation, difficulty in getting out of bed and were more likely to have discharge preferences not adequately considered.
End-of-Life Care
Modification of end-of-life practices has been one of the most psychologically distressing consequences of strict visitor policies. Cook and colleagues found that during the first wave of the COVID-19 pandemic only 44% of patients had a family member physically present in their room at the end-of-life (compared to 87% of patients in pre-pandemic times).33 Otani and colleagues found that a dying patient’s inability to say goodbye to family was associated with complicated grief on the part of the family.34 In a study of 1,058 health care providers across 21 ICUs in France, deep regret about the COVID-19 visiting restrictions was expressed, and led to symptoms of anxiety and/or depression.35
Labour and Delivery
Continual presence of family or a designated support person during labour has been associated with more favourable outcomes.36,37 Prior data has demonstrated that the continual presence of family or a designated support person during labour is associated with more favourable delivery outcomes and fewer medical and surgical interventions.36 Their absence is a risk factor for increased acute stress, birth trauma, and post-partum post-traumatic stress disorder.37,38 Appendix B provides a detailed overview of these studies.
The term visitor needs to distinguish between “social visitors” and “essential caregivers”. Family and essential caregivers are active and essential in the ongoing care of a patient admitted to hospital.
Safely Introducing Family and Essential Caregivers to the Bedside
A clear and transparent process for appointing a family/essential caregiver by the patient should be established. The degree of risk to each individual inpatient in the absence of family/essential caregiver exists on a continuum, based upon their specific clinical circumstances. Patient populations at high risk of harm from the absence of family/essential caregivers must be identified. The most studied populations demonstrating potential harms include, but are not limited to (1) patients with cognitive impairment or special care needs, (2) patients with, or at risk of, delirium, (3) patients with communication barriers, (4) obstetrical patients, (5) critically ill patients, (6) patients with unique sociocultural needs, and (7) patients at the end-of-life. Risk assessments must balance both the SARS-CoV-2 infection risk to the patient being visited, all in-patients on the unit, and family/essential caregivers against the risk to patient and increased work of health care providers in the absence of family/essential caregivers. Blanket policies should be avoided and exceptions for unique circumstances permitted (Table 1). The substantial between-jurisdiction variation in the prevalence of COVID-19 means that risk assessments should be made considering regional or hospital level conditions and visitor policies should be tailored accordingly.
Visitor policies need to be dynamic and iterative given the changing epidemiology to ensure integration of the most up-to-date knowledge when dealing with a novel virus and considering PPE supplies. While these policies may change and become more restrictive as the risk to patients and health care workers increases (i.e., increased prevalence of VOCs, hospital outbreaks, health care systems overwhelmed); the highest-risk patient populations should have exceptions granted. Given the likelihood of evolution of any hospital’s visitor policies over the subsequent few months, clear and effective policies need to be readily available. Furthermore, timely and transparent appeals processes need to be developed and implemented at a hospital level to process exemptions. A proposed framework is outlined in Figure 1.
Policies that could help to reduce the risk associated with family/essential caregivers during a pandemic include vaccines, enhanced screening, enhanced education, limiting the number of family/essential caregivers allowed to visit a patient during their admission, limiting the duration of visits, having a dedicated location for family/essential caregivers to eat/drink, and ensuring appropriate PPE (Figure 1).
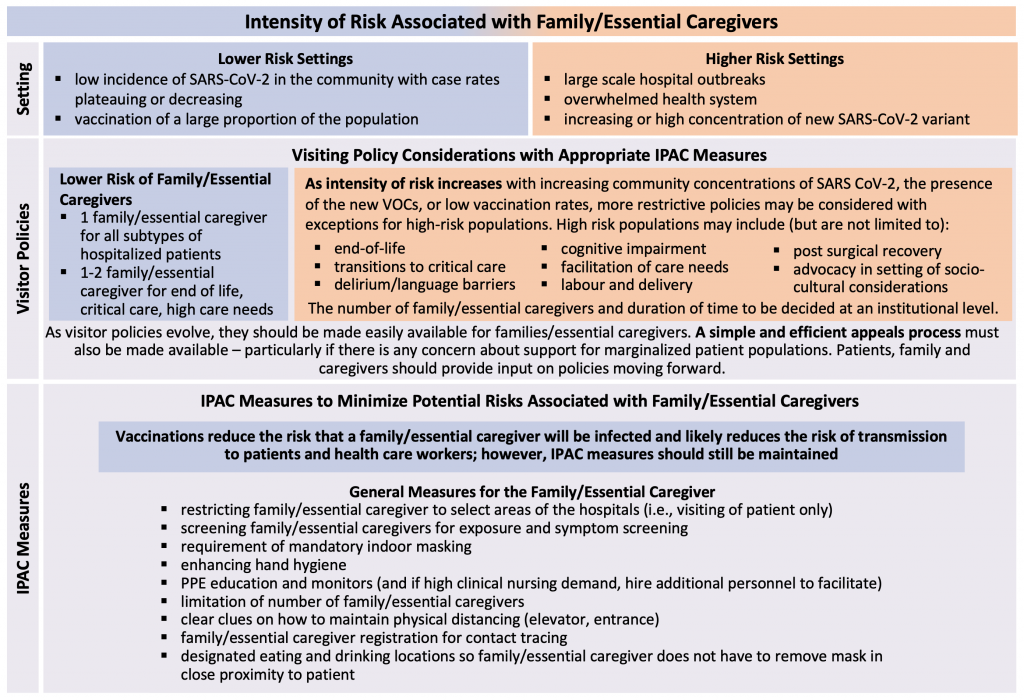
The proposed framework is for family and essential caregiver visitors only, not social visitors for adult in-patients.
Mechanisms to Mitigate Harms Associated with Family/Essential Caregiver Absence and Strict Visiting Policies
Occasionally, more restrictive visitor policies may need to be adopted (e.g., hospital outbreak, overwhelmed hospital system, lack of PPE) in order to protect family/essential caregivers, patients, and health care workers. In these settings exceptions should be considered for high-risk patient populations. We evaluated the literature for methods to enhance communication in the absence of in-person visitors. Two vital areas of communication during an inpatient admission include (1) connecting health care teams with families and (2) connecting patients with families.
Connecting with the Health Care Team
Close communication between families of acutely ill patients has been shown to improve psychological outcomes and lead to higher quality surrogate decision making surrounding the direction of care.39,40 Electronic communication through phone calls or video conferencing was widely adopted by health care systems during the COVID-19 pandemic.28A study that evaluated the feasibility and acceptability of electronic communication for palliative care family meetings found that 80% of family members felt comfortable articulating questions and expressing thoughts throughout the meeting.41 In one study, telephone communication was useful for sharing brief updates but were not ideal for more complex discussions surrounding goals of care. Video conferencing, when in person meetings were not feasible, were preferrable methods of communicating to ensure family and clinician perspectives were aligned.42 Videoconferencing may additionally facilitate the presence of translators where needed. However, this format of communication may not be culturally appropriate for all populations and warrants further evaluation. More data is needed to better quantify the effectiveness of these formats of communication across all care settings.
Effective, timely, and uninterrupted communication with each family may not be feasible during a pandemic given many competing time pressures. Family medical communication teams (FMCT), composed of allied health providers and physicians not participating directly in clinical care, are a unique approach to facilitating communication when health care providers may be overstretched. The FMCT model, implemented by Wendel and colleagues provided a 24-hour per day/7 days per week liaison service to support families of patients admitted to the ICU.43 This model was associated with (1) an improved transfer of information, (2) reduced fear that their loved one was alone, and (3) provided FMCT members a sense of renewed purpose during the pandemic.
Connecting Patients to Families
Telephone and video-communication has been reported to be an effective alternative way to connect patients to families in the setting of restricted visiting. In a study by Pun and colleagues that demonstrated a lower incidence of delirium across COVID-ICU patients who experienced family visitations, approximately half of these visits were conducted virtually.31 However, video conferencing requires access to devices and access tends to follow socioeconomic lines with related equity considerations.25,44 In the study by Piscitello and colleagues, there were more documented telephone and electronic communication meetings for White or African-American patients compared to those who were Hispanic or Latinx.25 Furthermore, there is concern about the increased workload it may create for nursing staff who may need to be present to facilitate communication, as well as important privacy implications.33 Certain jurisdictions adopted the use of e-communication teams (medical student or allied health providers) who would coordinate and facilitate e-communication between patients and families, or provide companionship for patients in circumstances where they would otherwise die alone.45,46 Techniques described to enhance the effectiveness of e-communication while maintaining privacy are outlined in Figure 2.
Without broad access or dedicated communication teams, electronic communication may be inconsistent, and may be limited by barriers such as knowledge of technology especially with older individuals. Where feasible, some centres have used outdoor spaces to facilitate visits between patients and families. Finally, electronic communication cannot replace the essential care often provided by caregivers at the bedside. See Appendix C for further details.
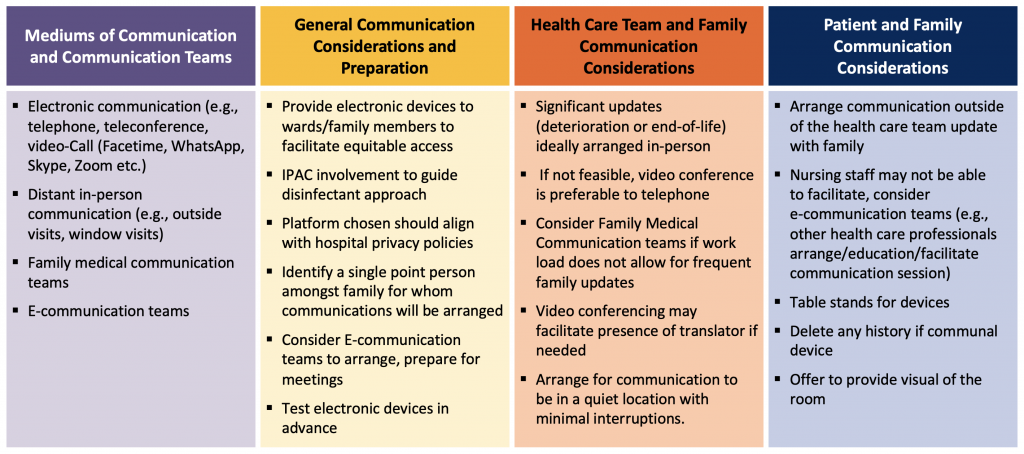
Culturally appropriate forms of communication need to be further evaluated and developed through engagement with different cultural leaders. The effectiveness of mediums of communication should be re-evaluate through feedback from patients, families, and caregivers.
Interpretation
Existing literature does not support any scenario where a complete restriction of family/essential caregivers across all patient subtypes from hospitals is required. It is essential that a distinction is made between general visitors and essential caregivers. Many institutions in Canada have adopted less restrictive policies in specific settings (e.g., critical care units) recognizing the importance of family/essential caregivers in the second and third wave of the pandemic after reflecting upon their experience in the first wave. However, the relaxation of restrictions has not been consistent across health care institutions, hospital departments, or at-risk groups. More data is needed surrounding its impact across different racialized communities and the acceptability of the different forms of electronic communication across different cultural groups.
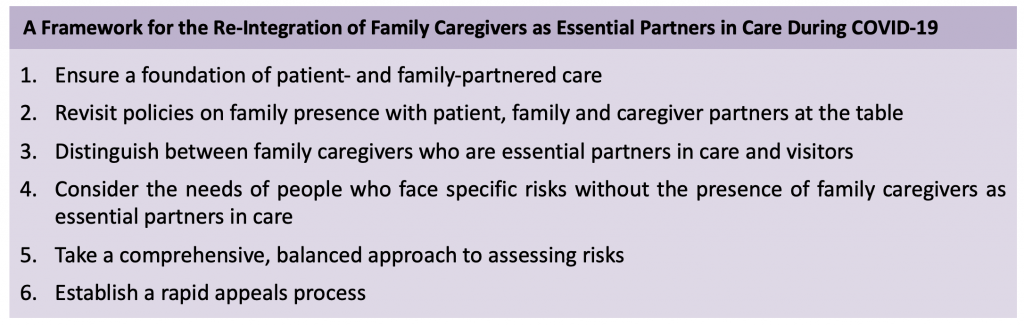
Table adapted from the Canadian Foundation for Healthcare Improvement.16
Future policies must incorporate the insight of patients, families, and essential caregivers. Robust data are needed to answer questions of competing risks of viral transmission, particularly with the increasing prevalence of VOCs and visitor restrictions across regions with varying community prevalence of SARS-CoV-2. These evaluations should specifically distinguish between essential caregivers and general visitors. A transparent and clear process of identifying family/essential caregivers is needed. Further evaluation of restrictions across different hospital departments (e.g., emergency departments, psychiatry, surgery) is needed to quantify the risk of visitor absence in specific settings.
A framework has been established by the Canadian Foundation for Healthcare Improvement for consideration in future policies (Table 2).1 While the literature has demonstrated the feasibility and acceptability of electronic forms of communication – not all populations are represented in this literature which warrants further evaluation. The literature may also be subject to publication bias by only reporting favourable experiences. An ongoing study by Fiest and colleagues is currently underway and will shed light on the implications of Canada’s visitor policies.47
We are only starting to understand the ramifications of strict visitor policies during the COVID-19 pandemic. Importantly, a distinction between essential caregivers – who are essential care partners – and general visitors is needed. With additional knowledge surrounding VOCs, and the impact of COVID-19 vaccinations, we have an opportunity to re-evaluate our practices and reflect upon our experiences. More data is needed to quantify the risk of general visitors vs. essential caregivers and the risks to the patient and burden on health care workers in the absence of essential caregivers. A comprehensive and balanced approach to assessing risk for future policies is needed with patient, family/essential caregivers at the table.
Methods Used for This Science Brief
The COVID-19 Evidence Synthesis Network performed a research evidence scan for this Science Brief, published in an Evidence Synthesis Briefing Note. The COVID-19 Evidence Synthesis Network is comprised of organizations in Ontario’s evidence synthesis and knowledge translation community who collectively provide high-quality, relevant, and timely synthesized research evidence about COVID-19. The methods for the evidence scan can be found in the methods section of the Briefing Note. The evidence scan was last updated on September 24, 2020.48
Public Health Ontario library services performed a search across MEDLINE, Ovid Embase, and EBSCOhost CINAHL using terms relevant to COVID-19, hospitals, and visitor policies and restrictions limited to English language and non-animal studies. All relevant articles were reviewed for their relevance to this Science Brief. The search was last updated on February 3, 2021.
References
- Canadian Foundation for Healthcare Improvement. Better Together: Re-Integration of Family Caregivers as Essential Partners in Care in a Time of COVID-19. Canadian Foundation for Healthcare Improvement; 2020. https://www.cfhi-fcass.ca/docs/default-source/itr/tools-and-resources/bt-re-integration-of-family-caregivers-as-essential-partners-covid-19-e.pdf?sfvrsn=5b3d8f3d_2
- Healthcare Excellence Canada. Re-integration of family caregivers as essential partners in care in a time of COVID-19. cfhi-fcass.ca. Published July 8, 2020. https://www.cfhi-fcass.ca/about/news-and-stories/news-detail
- The Honourable Mr. Justice Archie Campbell. The SARS commission report. Published January 9, 2007. http://www.archives.gov.on.ca/en/e_records/sars/index.html
- Creutzfeldt CJ, Schutz REC, Zahuranec DB, Lutz BJ, Curtis JR, Engelberg RA. Family presence for patients with severe acute brain injury and the influence of the COVID-19 pandemic. J Palliat Med. 2020;24(5):743-746.https://doi.org/10.1089/jpm.2020.0520
- Cattelan J, Castellano S, Merdji H, et al. Psychological effects of remote-only communication among reference persons of ICU patients during COVID-19 pandemic. J Intensive Care. 2021;9(1):5. https://doi.org/10.1186/s40560-020-00520-w
- Norton A, Wilson T, Geller G, Gross MS. Impact of hospital visitor restrictions on racial disparities in obstetrics. Health Equity. 2020;4(1):505-508. https://doi.org/10.1089/heq.2020.0073
- Artiga S, Orgera K, Pham O, Corallo B. Growing data underscore that communities of color are being harder hit by COVID-19. KFF. Published April 21, 2020. https://www.kff.org/policy-watch/growing-data-underscore-communities-color-harder-hit-covid-19/
- Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N. Outcomes of patient- and family-centered care interventions in the ICU: A systematic review and meta-analysis. Crit Care Med. 2017;45(10):1751-1761. https://doi.org/10.1097/CCM.0000000000002624
- Healthcare Excellence Canada. Much More than Just a Visit: A Review of Visiting Policies in Select Canadian Acute Care Hospitals. Canadian Foundation for Healthcare Improvement; 2015. https://www.cfhi-fcass.ca/innovations-tools-resources/item-detail
- Passarelli VC, Faico-Filho K, Moreira LVL, et al. Asymptomatic COVID-19 in hospital visitors: The underestimated potential of viral shedding. Int J Infect Dis. 2021;102:412-414. https://doi.org/10.1016/j.ijid.2020.10.057
- Bianco A, Buckley AB, Overbey J, et al. Testing of patients and support persons for Coronavirus disease 2019 (COVID-19) infection before scheduled deliveries. Obstet Gynecol. 2020;136(2):283-287.https://doi.org/10.1097/AOG.0000000000003985
- Kain D, Stall NM, Allen V, et al. Routine asymptomatic SARS-CoV-2 screen testing of staff in Ontario long-term care homes. Sci Briefs Ont COVID-19 Sci Advis Table. 2021;2(15). https://doi.org/10.47326/ocsat.2021.02.15.1.0
- Zhou Q, Gao Y, Wang X, et al. Nosocomial infections among patients with COVID-19, SARS and MERS: a rapid review and meta-analysis. Ann Transl Med. 2020;8(10). https://doi.org/10.21037/atm-20-3324
- Rhee C, Baker M, Vaidya V, et al. Incidence of nosocomial COVID-19 in patients hospitalized at a large US Academic Medical Center. JAMA Netw Open. 2020;3(9):e2020498. https://doi.org/10.1001/jamanetworkopen.2020.20498
- Wee LE, Conceicao EP, Sim JX-Y, Aung MK, Venkatachalam I. The impact of visitor restrictions on health care-associated respiratory viral infections during the COVID-19 pandemic: Experience of a tertiary hospital in Singapore. Am J Infect Control. 2021;49(1):134-135. https://doi.org/10.1016/j.ajic.2020.11.006
- Nassar Junior AP, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: A systematic review and meta-analysis. Crit Care Med. 2018;46(7):1175-1180.https://doi.org/10.1097/CCM.0000000000003155
- S. Department of Health & Human Services. New HHS Data Shows Major Strides Made in Patient Safety, Leading to Improved Care and Savings. Centers for Medicare & Medical Services; 2014. Accessed May 14, 2021. https://innovation.cms.gov/files/reports/patient-safety-results.pdf
- Canadian Foundation for Healthcare Improvement. Better together: e-integration of family caregivers as essential partners in care in a time of COVID-19. Published online July 2020. Accessed July 8, 2020. https://www.cfhi-fcass.ca/docs/default-source/itr/tools-and-resources/bt-re-integration-of-family-caregivers-as-essential-partners-covid-19-e.pdf?sfvrsn=5b3d8f3d_2
- United Nations Sustainable Development Group. Policy Brief: COVID-19 and the Need for Action on Mental Health. United Nations Sustainable Development Group; 2020. https://unsdg.un.org/sites/default/files/2020-05/UN-Policy-Brief-COVID-19-and-mental-health.pdf
- Public Health Agency of Canada. COVID-19 and people with disabilities in Canada. Government of Canada. Published November 24, 2020. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/people-with-disabilities.html
- Bélanger L, Bussières S, Rainville F, Coulombe M, Desmartis M. Hospital visiting policies – impacts on patients, families and staff: A review of the literature to inform decision making. J Hosp Adm. 2017;6(6):51. https://doi.org/10.5430/jha.v6n6p51
- DuPree E, Fritz-Campiz A, Musheno D. A new approach to preventing falls with injuries. J Nurs Care Qual. 2014;29(2):99-102. https://doi.org/10.1097/NCQ.0000000000000050
- Lomiguen CM, Rosete I, Chin J. Providing culturally competent care for COVID-19 intensive care unit delirium: A case report and review. Cureus. 2020;12(10). https://doi.org/10.7759/cureus.10867
- Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. 2017;171(4):372-381. https://doi.org/10.1001/jamapediatrics.2016.4812
- Piscitello GM, Fukushima CM, Saulitis AK, et al. Family meetings in the intensive care unit during the Coronavirus disease 2019 pandemic. Am J Hosp Palliat Med. 2021;38(3):305-312. https://doi.org/10.1177/1049909120973431
- Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382(23):2268-2270. https://doi.org/10.1056/NEJMc2008597
- Helms J, Kremer S, Merdji H, et al. Delirium and encephalopathy in severe COVID-19: a cohort analysis of ICU patients. Crit Care. 2020;24(1):491. https://doi.org/10.1186/s13054-020-03200-1
- Pun BT, Badenes R, Calle GHL, et al. Prevalence and risk factors for delirium in critically ill patients with COVID-19 (COVID-D): a multicentre cohort study. Lancet Respir Med. 2021;9(3):239-250. https://doi.org/10.1016/S2213-2600(20)30552-X
- Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291(14):1753-1762. https://doi.org/10.1001/jama.291.14.1753
- Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293-1304. https://doi.org/10.1056/NEJMoa1011802
- Kandori K, Okada Y, Ishii W, Narumiya H, Maebayashi Y, Iizuka R. Association between visitation restriction during the COVID-19 pandemic and delirium incidence among emergency admission patients: a single-center retrospective observational cohort study in Japan. J Intensive Care. 2020;8(1):90. https://doi.org/10.1186/s40560-020-00511-x
- Zeh RD, Santry HP, Monsour C, et al. Impact of visitor restriction rules on the postoperative experience of COVID-19 negative patients undergoing surgery. Surgery. 2020;168(5):770-776. https://doi.org/10.1016/j.surg.2020.08.010
- Cook DJ, Takaoka A, Hoad N, et al. Clinician perspectives on caring for dying patients during the pandemic. Ann Intern Med. 2020;174(4):493-500. https://doi.org/10.7326/M20-6943
- Otani H, Yoshida S, Morita T, et al. Meaningful communication before death, but not present at the time of death itself, is associated with better outcomes on measures of depression and complicated grief among bereaved family members of cancer patients. J Pain Symptom Manage. 2017;54(3):273-279. https://doi.org/10.1016/j.jpainsymman.2017.07.010
- Azoulay E, Cariou A, Bruneel F, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19: A cross-sectional study. Am J Respir Crit Care Med. 2020;202(10):1388-1398. https://doi.org/10.1164/rccm.202006-2568OC
- Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;2017(7). https://doi.org/10.1002/14651858.CD003766.pub6
- Ayers S. Birth trauma and post-traumatic stress disorder: the importance of risk and resilience. J Reprod Infant Psychol. 2017;35(5):427-430. https://doi.org/10.1080/02646838.2017.1386874
- Mayopoulos GA, Ein-Dor T, Li KG, Chan SJ, Dekel S. Giving birth under hospital visitor restrictions: Heightened acute stress in childbirth in COVID-19 positive women. medRxiv. Published online December 7, 2020:2020.11.30.20241026. https://doi.org/10.1101/2020.11.30.20241026
- Hoad N, Swinton M, Takaoka A, et al. Fostering humanism: a mixed methods evaluation of the Footprints Project in critical care. BMJ Open. 2019;9(11):e029810. https://doi.org/10.1136/bmjopen-2019-029810
- Vanstone M, Sadik M, Smith O, et al. Building organizational compassion among teams delivering end-of-life care in the intensive care unit: The 3 Wishes Project. Palliat Med. 2020;34(9):1263-1273.https://doi.org/10.1177/0269216320929538
- Kuntz JG, Kavalieratos D, Esper GJ, et al. Feasibility and acceptability of inpatient palliative care e-family meetings during COVID-19 pandemic. J Pain Symptom Manage. 2020;60(3). https://doi.org/10.1016/j.jpainsymman.2020.06.001
- Kennedy NR, Steinberg A, Arnold RM, et al. Perspectives on telephone and video communication in the intensive care unit during COVID-19. Ann Am Thorac Soc. 2020;18(5):838-847. https://doi.org/10.1513/AnnalsATS.202006-729OC
- Wendel PK, Stack RJ, Chisholm MF, et al. Development of a communications program to support care of critically ill Coronavirus disease 2019 (COVID-19) patients. J Patient Exp. 2020;7(5):673-676. https://doi.org/10.1177/2374373520956865
- Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic disparities in patient use of telehealth during the Coronavirus disease 2019 surge. JAMA Otolaryngol Neck Surg. 2021;147(3):287.https://doi.org/10.1001/jamaoto.2020.5161
- Haire E, Brown H, Wiggins N. “Compassion outside of the box”: The role of allied healthcare professionals in providing a companion service for patients at the end of life during the COVID-19 pandemic. J Pain Symptom Manage. Published online November 30, 2020. https://doi.org/10.1016/j.jpainsymman.2020.11.027
- Hojat M, DeSantis J, Ney DB, DeCleene-Do H. Empathy of medical students and compassionate care for dying patients: An sssessment of “no one dies alone” program. J Patient Exp. 2020;7(6):1164-1168. https://doi.org/10.1177/2374373520962605
- Calgary Critical Care Research Network. COVID-19 research studies. Cumming School of Medicine. Published 2021. https://cumming.ucalgary.ca/research/calgary-critical-care-research-network/research/COVID-19
- McMaster Health Forum. COVID-19 Rapid Evidence Profile #19.; 2020. Accessed May 14, 2021.https://www.mcmasterforum.org/docs/default-source/covidend/rapid-evidence-profiles/covid-19-rep-19_visitor-policies_2020-09-28.pdf?sfvrsn=841556d5_2
Document Information & Citation
Author Contributions: LM and FR conceived the Science Brief. LM wrote the first draft of the Science Brief. All authors revised the Science Brief critically for important intellectual content and approved the final version.
Citation: Munshi L, Odutayo A, Evans GA, et al. Impact of Hospital Visitor Restrictions during the COVID-19 Pandemic. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;2(31). https://doi.org/10.47326/ocsat.2021.02.31.1.0
Author Affiliations: The affiliations of the members of the Ontario COVID-19 Science Advisory Table can be found at https://covid19-sciencetable.ca/.
Declarations of Interest: The declarations of interest of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners can be found at https://covid19-sciencetable.ca/. The declarations of interest of external authors can be found under Additional Resources.
Copyright: 2021 Ontario COVID-19 Science Advisory Table. This is an open access document distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided that the original work is properly cited.
The views and findings expressed in this Science Brief are those of the authors and do not necessarily reflect the views of all of the members of the Ontario COVID-19 Science Advisory Table, its Working Groups, or its partners.
